Abstract
Summary
Guidance is provided in a European setting on the assessment and treatment of postmenopausal women at risk from fractures due to osteoporosis.
Introduction
The International Osteoporosis Foundation and European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis published guidance for the diagnosis and management of osteoporosis in 2013. This manuscript updates these in a European setting.
Methods
Systematic reviews were updated.
Results
The following areas are reviewed: the role of bone mineral density measurement for the diagnosis of osteoporosis and assessment of fracture risk; general and pharmacological management of osteoporosis; monitoring of treatment; assessment of fracture risk; case-finding strategies; investigation of patients; health economics of treatment. The update includes new information on the evaluation of bone microstructure evaluation in facture risk assessment, the role of FRAX® and Fracture Liaison Services in secondary fracture prevention, long-term effects on fracture risk of dietary intakes, and increased fracture risk on stopping drug treatment.
Conclusions
A platform is provided on which specific guidelines can be developed for national use.
Similar content being viewed by others
Diagnosis of osteoporosis
-
1.
The operational definition of osteoporosis is based on the T-score for BMD assessed by DXA at the femoral neck or spine and is defined as a value for BMD 2.5 SD or more below the young female adult mean.
-
2.
For clinical purposes, other sites and techniques can be used for diagnosis.
-
3.
Low bone mass (osteopenia) should not be considered a disease category but is intended solely for purpose of epidemiological description.
Risk factors for fragility fractures
-
1.
Several factors contribute significantly to fracture risk over and above that provided by bone mineral density measurements. These include age, sex, low body mass index, previous fragility fracture, parental history of hip fracture, glucocorticoid treatment, current smoking, alcohol intake of 3 or more units daily and causes of secondary osteoporosis.
-
2.
Additional risk factors that are of use in case finding include height loss (> 4 cm) and thoracic kyphosis.
-
3.
Bone markers (serum procollagen type I N propeptide (s-PINP) and serum C-terminal cross-linking telopeptide of type I collagen (s-CTX) as markers of bone formation and bone resorption, respectively) have some prognostic significance for fracture in situations where BMD is unavailable.
Assessment of fracture risk
-
1.
Country-specific FRAX® should be used to assess fracture probability in postmenopausal women who have risk factors for fracture. In individuals at intermediate risk, bone mineral density (BMD) measurement should be performed using dual energy X-ray absorptiometry and FRAX fracture probability re-estimated.
-
2.
Where BMD testing is unavailable, FRAX can be used without the input of BMD
-
3.
Trabecular bone score (TBS) may be used as an adjunct to BMD measurements and FRAX.
-
4.
Interpretation of FRAX scores may be influenced by exposure to glucocorticoids, information on lumbar spine BMD, trabecular bone score, hip axis length, falls history, immigration status and type 2 diabetes mellitus.
-
5.
Vertebral fracture assessment should be considered if there is a history of ≥ 4 cm height loss, kyphosis, recent or current long-term oral glucocorticoid therapy or a BMD T-score ≤ − 2.5.
Lifestyle and dietary measures
-
1.
Recommendations should include a daily calcium intake of between 800 and 1200 mg and sufficient dietary protein, ideally achieved through dairy products.
-
2.
A daily dose of 800 IU cholecalciferol should be advised for postmenopausal women at increased risk of fracture.
-
3.
Calcium supplementation is appropriate if the dietary intake is below 800 mg/day, and vitamin D supplementation considered in patients at risk of, or showing evidence of, vitamin D insufficiency.
-
4.
Regular weight-bearing exercise should be advised, tailored to the needs and abilities of the individual patient.
-
5.
A history of falls should be obtained in individuals at increased risk of fracture with further assessment and appropriate measures undertaken in those at increased risk.
Pharmacological intervention in postmenopausal women
-
1.
The oral bisphosphonates (alendronate, risedronate and ibandronate) may be used as initial treatments in the majority of cases. In women intolerant to oral bisphosphonates (or in those for whom they are contraindicated), intravenous bisphosphonates or denosumab provide the most appropriate alternatives, with raloxifene, or menopause hormone therapy as additional options. Teriparatide is preferentially recommended for patients at high risk of fracture.
-
2.
Treatments should be reviewed after 3–5 years treatment with bisphosphonate. Fracture risk should be reassessed after a new fracture, regardless of when it occurs. The risk of new clinical and vertebral fractures increases in patients who stop treatment.
-
3.
Withdrawal of denosumab therapy is associated with a rebound in vertebral fracture rate. Bisphosphonate therapy can be considered after discontinuation of denosumab.
-
4.
There is little evidence to guide decision-making beyond 10 years of treatment and management options in such patients should be considered on an individual basis.
Intervention thresholds for pharmacological intervention
-
1.
The thresholds recommended for decision-making are based on probabilities of major osteoporotic and hip fracture derived from FRAX. These vary in different healthcare systems with variation in ‘willingness to pay’.
-
2.
Women aged over 65 years with a prior fragility fracture can be considered for treatment without the need for further assessment; BMD measurement may be felt more appropriate in younger postmenopausal women.
-
3.
Age-dependent intervention thresholds provide clinically appropriate and equitable access to treatment and have been shown to be cost-effective.
Systems of care
-
1.
The utility of age-dependent FRAX thresholds in population screening approach has recently been validated as feasible, effective and health economically viable.
-
2.
Coordinator-based Fracture Liaison Services (FLS) should be used to systematically identify men and women with fragility fracture. Their effectiveness and cost-effectiveness have been established recently.
Introduction
In 1997 The European Foundation for Osteoporosis and Bone Disease (subsequently the International Osteoporosis Foundation; IOF) published guidelines for the diagnosis and management of osteoporosis [1], subsequently updated in 2008 [2] and 2013 [3] by the IOF and European Society for Clinical and Economic Evaluation of Osteoporosis and Osteoarthritis (ESCEO). The scope of the present guideline is to review and update the assessment and diagnosis of osteoporosis, the therapeutic interventions available and the manner in which these can be used to develop management strategies for the prevention of fragility fracture in postmenopausal women. The guideline is intended for all healthcare professionals involved in the management of osteoporosis. Where available, systematic reviews, meta-analyses and randomised controlled trials have been used to provide the evidence base. The evidence base was updated using PubMed to identify systematic reviews and meta-analyses from January 2008 to December 2017. The recommendations in this guideline were endorsed by the Scientific Advisory Board of ESCEO and the Committee of Scientific Advisors and the Committee of National Societies of the IOF.
The high societal and personal costs of osteoporosis pose challenges to public health and physicians, particularly since most patients with osteoporosis remain untreated. There is a large gap between the number of women who are treated compared to the proportion of the population that could be considered eligible for treatment based on their fracture risk. In the European Union (EU), it is estimated that there are and 18.44 million women who have a fracture probability that equals or exceeds that of a woman with a prior fragility as assessed by FRAX® (i.e. individuals at or above a ‘fracture threshold’). On the conservative assumption that treatments are only given to patients at high risk, prescription data suggest that more than 57% of women at high risk do not receive bone-specific treatment [4]. Moreover, uptake of treatments for osteoporosis, particularly the bisphosphonates, has declined in recent years [5, 6]. In patients with fragility fractures, less than 20% of patients with a fragility fracture receive therapy to reduce future fracture within the year following fracture [7,8,9]. Against this sobering background, the aim of this guidance is to stimulate a cohesive approach to the management of osteoporosis in Europe. The term guidance rather than guidelines is used, to avoid any prescriptive connotations since country- or region-specific guidelines are now widely available in many European countries and continue to evolve. Rather, the guidance can inform the development of new guidelines or the revision of existing guidelines. Whilst focussed on a European perspective and on postmenopausal women, the principles may be of some assistance in other regions of the world and in men.
Osteoporosis in Europe
Osteoporosis is defined as a systemic skeletal disease characterised by low bone mass and microarchitectural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture [10]. Although the diagnosis of the disease relies on the quantitative assessment of bone mineral density, which is a major determinant of bone strength, the clinical significance of osteoporosis lies in the fractures that arise. Because a variety of non-skeletal factors contribute to fracture risk [11,12,13], the diagnosis of osteoporosis by the use of BMD measurements is at the same time an assessment of a risk factor for the clinical outcome of fracture. For these reasons, there is a distinction to be made between the use of BMD for diagnosis and for risk assessment.
Common sites for osteoporotic fracture are the spine, hip, distal forearm and proximal humerus. The remaining lifetime probability in women at the menopause of a fracture at any one of these sites exceeds that of breast cancer (approximately 12%), and the likelihood of a fracture at any of these sites is 40% or more in Western Europe [14] (Table 1), a figure close to the probability of coronary heart disease.
Fragility fractures are a major cause of morbidity in the population. Hip fractures cause acute pain and loss of function, and nearly always lead to hospitalisation. Recovery is slow, and rehabilitation is often incomplete, with many patients permanently institutionalised in nursing homes. Vertebral fractures may cause acute pain and loss of function but may also occur without serious symptoms. Vertebral fractures often recur, however, and the consequent disability increases with the number of fractures. Distal radial fractures also lead to acute pain and loss of function, but functional recovery is usually good or excellent.
In 2010, it was estimated that 22 million women and 5.5 million men in the EU had osteoporosis using the diagnostic criterion of the WHO [4]. The number of new fractures in 2010 in the EU was estimated at 3.5 million, comprising approximately 610,000 hip fractures, 520,000 vertebral fractures, 560,000 forearm fractures and 1,800,000 other fractures (i.e. pelvis, rib, humerus, tibia, fibula, clavicle, scapula, sternum and other femoral fractures). Two thirds of all incident fractures occurred in women. Among people age 50 years or more who were still alive in 2010, 3.3 million individuals had sustained a hip fracture (prevalence of prior hip fracture). The corresponding number of men and women with prior clinical vertebral fractures was estimated at 3.5 million. Due to changes in population demography, the annual number of fragility fractures will rise from 3.5 million in 2010 to 4.5 million in 2025, corresponding to an increase of 28%.
It is widely recognised that osteoporosis and the consequent fractures are associated with increased mortality, with the exception of forearm fractures [15]. In the case of hip fracture, most deaths occur in the first 3–6 months following the event, of which 20–30% is causally related to the fracture event itself [16]. In Sweden, the number of deaths that are causally related to hip fracture account for more than 1% of all deaths, somewhat higher than the deaths attributed to pancreatic cancer and somewhat lower than the deaths attributed to breast cancer [16]. In 2010, the number of deaths in the EU that were causally related to fractures was estimated at 43,000. Approximately 50% of fracture-related deaths in women were due to hip fractures, 28% to clinical vertebral and 22% to other fractures. Corresponding proportions for men were 47, 39 and 14%, respectively [4].
The total health burden, measured in terms of lost quality-adjusted life years (QALYs), was estimated at 1,180,000 QALYs for the EU. Twice as many QALYs were lost in women compared to men. The majority of the QALYs lost were a consequence of prior fractures. In Europe, osteoporosis accounted for more disability and life years lost (DALYs) than rheumatoid arthritis, but less than osteoarthritis. With regard to neoplastic diseases, the burden of osteoporosis was greater than for all sites of cancer, with the exception of lung cancers [17].
The cost of osteoporosis, including pharmacological intervention in the EU in 2010, was estimated at €37 billion. Costs of treating incident fractures represented 66% of these costs, pharmacological prevention 5% and long-term fracture care 29%. Excluding cost of pharmacological prevention, hip fractures represented 54% of the costs, ‘other fractures’ represented 39% and vertebral and forearm fractures represented 5 and 1%, respectively [4]. Assigning a QALY the value of 2xGDP, the total value of QALYs lost in 2010 was estimated at €61.4 billion.
Bone mineral measurements
The objectives of bone mineral measurements are to provide diagnostic criteria, prognostic information on the probability of future fractures, and a baseline on which to monitor the natural history of the treated or untreated patient. Bone mineral density (BMD) is the amount of bone mass per unit volume (volumetric density), or per unit area (areal density), and both can be measured in vivo by densitometric techniques.
A wide variety of techniques is available to assess bone mineral that are reviewed elsewhere [18,19,20,21]. The most widely used are based on X-ray absorptiometry in bone, particularly dual energy X-ray absorptiometry (DXA). Other techniques include quantitative ultrasound (QUS), quantitative computed tomography (QCT) applied both to the appendicular skeleton and to the spine, peripheral DXA, digital X-ray radiogrammetry, radiographic absorptiometry and other radiographic techniques. Other important determinants of bone strength for both cortical and trabecular bone include macro-and microarchitecture (e.g. cross-sectional moment of inertia, hip axis length, cortical thickness, finite element analysis, trabecular bone score, cortical porosity) [22,23,24,25,26,27].
DXA is the most widely used bone densitometric technique. It is versatile in the sense that it can be used to assess bone mineral density/bone mineral content of the whole skeleton as well as specific sites, including those most vulnerable to fracture [18]. Areal density (g/cm2) rather than a true volumetric density (g/cm3) is measured since the scan is two dimensional. Areal BMD accounts for about two thirds of the variance of bone strength as determined in vitro on isolated bones, such as the vertebral body or proximal femur. DXA can also be used to visualise lateral images of the spine from T4 to L4 to detect fractures of the vertebral bodies [28,29,30]. Vertebral fracture assessment (VFA) may improve fracture risk evaluation, since many patients with vertebral fracture may not have a BMD T-score classified as osteoporosis. This procedure involves less radiation and is less expensive than a conventional X-ray examination but performs comparably to traditional radiographs [31].
Whereas whole body bone, fat and lean mass can also be measured using DXA, these measurements are useful for research, but they do not assist in the routine diagnosis or assessment of osteoporosis.
The performance characteristics of many measurement techniques have been well documented [32, 33]. For the purpose of risk assessment and for diagnosis, a characteristic of major importance is the ability of a technique to predict fractures. This is traditionally expressed as the increase in the relative risk of fracture per standard deviation unit decrease in bone mineral measurement—termed the gradient of risk.
Limitations of BMD
There are a number of technical limitations in the general application of DXA for diagnosis, which should be recognised [34, 35]. The presence of osteomalacia, a complication of poor nutrition in the elderly, will underestimate total bone matrix because of decreased mineralisation of bone. Osteoarthrosis or osteoarthritis at the spine or hip are common in the elderly, and contribute to the density measurement, but not necessarily to skeletal strength. Heterogeneity of density due to osteoarthrosis, previous fracture or scoliosis can often be detected on the scan and in some cases excluded from the analysis. Some of these problems can be overcome with adequately trained staff and rigorous quality control.
Diagnosis of osteoporosis
Bone mineral density is most often described as a T-score or Z-score, both of which are units of standard deviation (SD). The T-score describes the number of SDs by which the BMD in an individual differs from the mean value expected in young healthy individuals. The operational definition of osteoporosis is based on the T-score for BMD [11, 34] assessed at the femoral neck and is defined as a value for BMD 2.5 SD or more below the young female adult mean (T-score less than or equal to − 2.5 SD) [3, 12, 36, 37]. The Z-score describes the number of SDs by which the BMD in an individual differs from the mean value expected for age and sex. It is mostly used in children and adolescents [38].
The reference range recommended by the IOF, ESCEO, ISCD, WHO and NOF for calculating the T-score [3, 12, 36, 37, 39] is the NHANES III reference database for femoral neck measurements in women aged 20–29 years [36]. Note that the diagnostic criteria for men use the same female reference range as that for women. This arises fortuitously because for any age and BMD at the femoral neck, the risk of hip fracture or a major osteoporotic fracture is approximately the same in men and women [40,41,42]. On GE Healthcare bone densitometers, there is an option for T-scores for men to be given relative to either the male or female reference range in DXA readouts. However, the T-score cannot be used interchangeably with different techniques and at different sites, since the prevalence of osteoporosis and proportion of individuals allocated to any diagnostic category would vary, as does the risk of fracture [39].
These considerations have led to the adoption of the femoral neck as the reference site [39], but do not preclude the use of other sites and technologies in clinical practice, though it should be recognised that the information derived from the T-score will differ from that provided by BMD at the femoral neck.
Measurement of multiple skeletal sites
A number of guidelines favour the concurrent use of BMD at the proximal femur and at the lumbar spine for patient assessment. Patients are defined as having osteoporosis on the basis of the lower of two T-scores [43, 44]. The prediction of fracture is, however, not improved overall using multiple sites [45,46,47]. Selection of patients on the basis of a minimum value from two or more tests will, however, increase the number of patients selected. The same result can be achieved by less stringent criteria for the definition of osteoporosis, by defining osteoporosis, for example, as a T-score of < − 2.0 SD rather than < − 2.5 SD. Notwithstanding, the measurement of more than one site can aid in the assessment of individuals (discussed below).
Low bone mass (osteopenia)
It is recommended that diagnostic criteria be reserved for osteoporosis and that low bone mass (osteopenia) should not be considered a disease category.
Prevalence of osteoporosis
Because the distribution of BMD in the young healthy population is normally distributed and bone loss occurs with advancing age, the prevalence of osteoporosis increases with age and thus depends on the demography of the population. The prevalence of osteoporosis in the 27 countries of the EU in men and women is shown in Table 2 [4]. Approximately 21% of women aged 50–84 years are classified as having osteoporosis accounting for more than 22 million women in these countries.
These data assume that the distribution of femoral neck BMD is the same in these index countries. There may be small differences in the age- and sex-specific BMD in different European countries as well as within countries. If so, these differences in BMD are relatively small [48] and insufficient to account for the observed differences in fracture rates (see below).
Risk factors for fracture
BMD
Assessment of BMD has provided a pivotal determinant of fracture risk and many guidelines have used BMD thresholds to determine whether treatments should be recommended. Intervention thresholds have ranged from T-scores of − 3 SD to − 1.5 SD depending on the clinical context, the country or on health economic factors. The use of bone mass measurements for prognosis depends upon accuracy. Accuracy in this context is the ability of the measurement to predict fracture. In general, all densitometric techniques have high specificity but low sensitivity, which varies with the cutoff chosen to designate high risk.
At the age of 50 years, for example, the proportion of women with osteoporosis who will fracture their hip, spine or forearm or proximal humerus in the next 10 years (i.e. positive predictive value) is approximately 45%. Despite this, the overall detection rate for these fractures (sensitivity) is low and 96% of fractures at the spine, hip, forearm or proximal humerus will occur in women without osteoporosis [49]. The low sensitivity is one of the reasons why widespread population-based screening with BMD is not widely recommended in women at the time of the menopause [11].
Many cross-sectional and prospective population studies indicate that the risk for fracture increases by a factor of 1.5 to 3.0 for each standard deviation decrease in bone mineral density [32]. There are, however, significant differences in the performance of different techniques at different skeletal sites. In addition, the performance depends on the type of fracture that one wishes to predict [30, 32, 50]. For example, BMD assessments by DXA to predict hip fracture are more predictive when measurements are made at the hip rather than at the spine or forearm (Table 3). For the prediction of hip fracture, the gradient of risk provided by hip BMD in a meta-analysis is 2.6 [32]. In other words, the fracture risk increases 2.6-fold for each SD decrease in hip BMD. Thus, an individual with a Z-score of − 3 SD at the hip would have a 2.63 or greater than 15-fold higher risk than an individual of the same age with a Z-score of 0. Where the intention is to predict any osteoporotic fracture, the commonly used techniques are comparable: The risk of fracture increases approximately 1.5-fold for each standard deviation decrease in the measurement so that an individual with a measurement of 3 standard deviations below the average value for age would have a 1.53 or greater than 3-fold higher risk than an individual with an average BMD. Note that the risk of fracture in individuals with an average BMD is lower than the average fracture risk, since fracture risk is a convex function of BMD.
The performance characteristics of quantitative ultrasound are similar. Most studies suggest that measurements of broadband ultrasound attenuation or speed of sound at the heel are associated with a 1.5- to 2-fold increase in risk for each standard deviation decrease in the measured variable [33, 51]. Comparative studies indicate that these gradients of risk are very similar to those provided by peripheral assessment of bone mineral density at appendicular sites by absorptiometric techniques to predict any osteoporotic fracture [32]. Unlike DXA, however, the long-term predictive value wanes with time [52]. Note also that the WHO criteria for the diagnosis of osteoporosis cannot be applied to ultrasound results.
Clinical risk factors
A large number of risk factors for fracture have been identified [53,54,55]. For the purposes of improving risk assessment, interest lies in those factors that contribute significantly to fracture risk over and above that provided by bone mineral density measurements or age [56]. A good example is age. For any BMD, fracture risk is much higher in the elderly than in the young [57]. This is because age contributes to risk independently of BMD. At the threshold for osteoporosis (T-score = − 2.5 SD), the 10-year probability of hip fracture ranges 5-fold in women from Sweden depending on age (Fig. 1) [49]. Thus, the consideration of age and BMD together increases the range of risk that can be identified.
Ten-year probability of hip fracture in women from Sweden according to age and T-score for femoral neck BMD [49], with kind permission from Springer Science and Business Media
Over the past few years, a series of meta-analyses have been undertaken to identify additional clinical risk factors that could be used in case-finding strategies, with or without the use of BMD [12]. There are a number of factors to be considered in the selection of risk factors for case finding. Of particular importance in the setting of primary care is the ease with which they might be used. For a globally applicable tool, the chosen risk factors should also be valid in an international setting and their predictive value documented over time. A further and critical consideration is the reversibility of risk, i.e. is there evidence that the risk identified by a risk factor is amenable to therapeutic intervention (reversibility of risk—not reversible risk). Age is an example of an irreversible risk factor, but the risk of fracture identified by age has reversibility. The risk factors that are used for clinical assessment with FRAX are summarised in Table 4 [12, 41, 58,59,60,61,62,63,64]. Each of these risk factors has been shown to identify reversibility of risk [65].
In the case of causes of secondary osteoporosis, the increase in fracture risk is presumed to be mediated by low BMD. The exceptions are glucocorticoid exposure and rheumatoid arthritis for which risks have been identified that are independent of BMD. A further candidate is type 2 diabetes mellitus since recent evidence suggests an important independent risk [66,67,68].
It should be noted that falls risk is not included in Table 4, though it has been used in some risk engines [69, 70], since the risk of fracture that is identified may not be associated with reversibility of risk. For example, patients selected on the basis of risk factors for falling may respond less to agents that preserve bone mass than those selected on the basis of low BMD [71].
Biochemical assessment of fracture risk
Bone markers are increased after the menopause, and in several studies the rate of bone loss varies according to the marker value [72]. Thus, a potential clinical application of biochemical indices of skeletal metabolism is in assessing fracture risk. The IOF and International Federation of clinical Chemistry and Laboratory Medicine (IFCC) have proposed two of several markers as reference analytes in the prediction of fracture risk; serum procollagen type I N propeptide (s-PINP) and serum C-terminal cross-linking telopeptide of type I collagen (s-CTX) as markers of bone formation and bone resorption, respectively [73]. A meta-analysis of prospective studies showed a significant association between s-PINP and the risk of fracture. The hazard ratio per SD increase in s-PINP (gradient of risk; GR) was 1.23 (95% CI 1.09–1.39) for men and women combined unadjusted for bone mineral density. There was also a significant association between s-CTX and risk of fracture GR = 1.18 (95% CI 1.05–1.34) unadjusted for bone mineral density. For the outcome of hip fracture, the association between s-CTX and risk of fracture was slightly higher, 1.23 (95% CI 1.04–1.47) [74]. Thus, there is a modest but significant association between these markers and the future risk of fractures. Currently, there are efforts by IFCC and IOF to harmonise markers of bone turnover, which, if successful, may promote markers of bone turnover for fracture risk prediction [75].
Trabecular bone score
Trabecular bone score (TBS) is a recently developed analytical tool that performs novel grey-level texture measurements on lumbar spine DXA images, and thereby captures information relating to trabecular microarchitecture. Low TBS is consistently associated with an increase in both prevalent and incident fractures that is partly independent of both clinical risk factors and areal BMD at the lumbar spine and proximal femur [23, 76]. It can thus be used as an adjunct to BMD measurements and is a software option for densitometers. Studies including a meta-analysis have shown an incremental improvement in fracture prediction when lumbar spine TBS is used in combination with FRAX variables [77,78,79,80,81]. In the meta-analysis, when additionally adjusted for FRAX 10-year probability of major osteoporotic fracture, TBS remained a significant, independent predictor for fracture (Gradient of risk = 1.32, 95% CI 1.24–1.41) [77]. The adjustment of FRAX probability for TBS resulted in a small increase in the GR (1.76, 95% CI 1.65–1.87 versus 1.70, 95% CI 1.60–1.81). A smaller change in GR for hip fracture was observed (FRAX® hip fracture probability GR 2.25 vs. 2.22). Thus, TBS is a predictor of fracture risk independently of FRAX and supports the use of TBS to adjust for FRAX probability. Adjustment of FRAX probabilities [77] is available from a dedicated web site (https://www.sheffield.ac.uk/TBS/CalculationTool.aspx) or via the FRAX web site (see Fig. 2).
Screen page for input of data and format of results in the UK version of the FRAX® tool (UK model, version 3.5. http://www.shef.ac.uk/FRAX). [With permission of the Centre for Metabolic Bone Diseases, University of Sheffield Medical School, UK]
TBS may also have a role in the assessment of fracture risk in some causes of secondary osteoporosis (e.g. diabetes, hyperparathyroidism and glucocorticoid-induced osteoporosis).
Vertebral fracture assessment
The majority of vertebral fractures do not come to medical attention and thus remain undiagnosed [82]. Moderate or severe vertebral fractures, even when asymptomatic, are strong risk factors for subsequent fracture at the spine and other skeletal sites [83, 84]. Vertebral fracture assessment should therefore be considered in high-risk individuals, using either lateral lumbar and thoracic spine radiographs or lateral spine DXA imaging. Vertebral fracture assessment should be considered in postmenopausal women if there is a history of ≥ 4 cm height loss, kyphosis, recent or current long-term oral glucocorticoid therapy, or a BMD T-score ≤ − 2.5. It should also be considered in individuals with a history of non-vertebral fracture [85].
Assessment of fracture risk
Whereas assessment guidelines have traditionally been based on BMD, its limitations have stimulated the development of risk engines that integrate several risk factors for fracture [86]. These include the Garvan fracture risk calculator [69], QFracture® [70] and FRAX® [12, 87]. Of these, FRAX has been the most extensively used. Since its release in 2008, models have been made available for 64 countries in 34 languages, covering 80% of the world population. The website (http://www.shef.ac.uk/FRAX) receives approximately 6 million visits annually and in 2012–2013 calculations arose from 173 countries [88]. This underestimates considerably the uptake of FRAX because the website is not the sole portal for the calculation of fracture probabilities. For example, FRAX is available in BMD equipment, on smartphones, and, in some countries, through hand-held calculators. FRAX has been incorporated into more than 80 guidelines worldwide [89].
Introduction to FRAX
FRAX® is a computer-based algorithm that calculates the 10-year probability of a major fracture (hip, clinical spine, humerus or wrist fracture) and the 10-year probability of hip fracture [12].
Fracture risk is calculated from age, body mass index and dichotomized risk factors comprising prior fragility fracture, parental history of hip fracture, current tobacco smoking, ever use of long-term oral glucocorticoids, rheumatoid arthritis, other causes of secondary osteoporosis and alcohol consumption (Fig. 2). Femoral neck BMD can be optionally input to enhance fracture risk prediction [90]. Fracture probability is computed taking both the risk of fracture and the risk of death into account. The use of clinical risk factors in conjunction with BMD and age improves sensitivity of fracture prediction without adverse effects on specificity [90].
Fracture probability differs markedly in different regions of the world [91]. The heterogeneity in Europe is shown in Fig. 3. For this reason, FRAX is calibrated to those countries where the epidemiology of fracture and death is known (currently 64 countries).
Ten-year probability (%) of a major osteoporotic fracture in women from different European countries. BMI set to 25 kg/m2. Data from http://www.shef.ac.uk/FRAX
Limitations of FRAX
The limitations of FRAX have been reviewed recently [89]. The FRAX assessment takes no account of dose-responses for several risk factors. For example, two prior fractures carry a much higher risk than a single prior fracture [92]. Dose-responses are also evident for glucocorticoid exposure [93], cigarette smoking [61] and alcohol intake [60]. Since it is not possible to accommodate all such scenarios with the FRAX algorithm, these limitations should temper clinical judgement.
A history of falls is a significant risk factor for fracture but is not incorporated into the FRAX model. Moreover, a significant risk of fracture remains after adjusting for FRAX [94]. However, the incorporation of falls into FRAX is problematic for several reasons. First, at the time of the release of FRAX, existing falls data were not of adequate quality, including the heterogeneous construct of questions on falls. Second, falls risk is inherently taken into account in the algorithm, though not as an input variable [95]. Thus, the fracture probability given for any combination of risk factors assumes that the falls risk is that observed (but not documented) in the cohorts used to construct FRAX. Third, the interrelationship of falls risk with the other FRAX variables has been inadequately explored on an international basis. Fourth, the relationship between the risk variable and mortality needs to be accounted for, but there are no data available. These technical problems aside, risk assessment tools are intended to identify a risk that is amenable to a therapeutic intervention. However, falls as a risk variable do not consistently pass the test of reversibility of risk [71, 96,97,98], a necessary feature of any risk variable used in tools to direct interventions [12, 65, 99].
To address some of these and other limitations, relatively simple arithmetic adjustments have been proposed, which can be applied to conventional FRAX estimates of probabilities of hip fracture and a major fracture to adjust the probability assessment with knowledge of:
With regard to glucocorticoids, Table 5 summarises the manner in which FRAX estimates of probabilities of hip fracture and a major osteoporotic fracture can be adjusted with knowledge of the dose of glucocorticoids [100]. For example, a woman aged 60 years from the UK taking glucocorticoids for rheumatoid arthritis (no other risk factors and BMI of 24 kg/m2) has a 10-year probability for a major fracture of 13%. If she is on a higher than average dose of prednisolone (> 7.5 mg daily), then the revised probability should be 15% (13 × 1.15).
Lumbar spine BMD is frequently measured by DXA and indeed is incorporated into several clinical guidelines. It is the site favoured for monitoring treatment and there is thus much interest in the implications for FRAX of measurements at the lumbar spine, since there are situations where there is a large discordance in the T-score at different skeletal sites in individuals for whom the use of this information will enhance the accuracy for the characterisation of risk, particularly if they lie close to an intervention threshold. The impact of spine/femoral neck T-score discordance has been explored in a large BMD-referral population from Manitoba, Canada. There was approximately a 10% change in fracture risk for each unit of T-score discordance [101]. On this basis, the clinician may increase/decrease FRAX estimate for a major fracture by one-tenth for each rounded T-score difference between the lumbar spine and femoral neck.
Additionally, FRAX values have been shown to be largely unaffected by socioeconomic status [108], variation in body composition [109] and a concern that treatment might invalidate the interpretation of FRAX appears misplaced [110].
Assessment of risk
At present there is no universally accepted policy for population screening in Europe to identify patients with osteoporosis or those at high risk of fracture. With the increasing development of effective agents and price reductions, this view may change, particularly for elderly people [111, 112]. In the absence of a screening policy, patients are identified opportunistically using a case-finding strategy on the finding of a previous fragility fracture or the presence of significant risk factors. The risk factors that are used for clinical assessment, summarised in Table 4, may be used but in principle any risk factor that alerts the physician to the possibility of osteoporosis is a candidate. Examples are height loss (> 4 cm) [113], thoracic kyphosis and the many other less well-characterised causes of secondary osteoporosis.
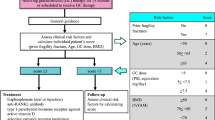
A general approach to risk assessment is shown in Fig. 4 [114]. The process begins with the assessment of fracture probability and the categorisation of fracture risk on the basis of age, sex, BMI and the clinical risk factors. On this information alone, some patients at high risk may be considered for treatment without recourse to BMD testing. For example, many guidelines in Europe [1, 89, 114] recommend treatment in the absence of information on BMD in women with a previous fragility fracture (a prior vertebral or hip fracture in North America) [115, 116]. Many physicians would also perform a BMD test, but frequently this is for reasons other than to decide on intervention, for example, as a baseline to monitor treatment. There will be other instances where the probability is so low that a decision not to treat can be made without BMD. Thus, not all individuals require a BMD test. The size of the intermediate category in Fig. 4 will vary in different countries. In countries that provide reimbursement for DXA, this will be a large category, whereas in a large number of countries with limited or no access to densitometry, the size of the intermediate group will necessarily be small. In other countries (e.g. the UK), where provision for BMD testing is sub-optimal [117], the intermediate category will lie between the two extremes.
Management algorithm for the assessment of individuals at risk of fracture [114], with kind permission from Springer Science and Business Media
Intervention thresholds
Whereas BMD provides the cornerstone for the diagnosis of osteoporosis, the use of BMD alone is less than optimal as an intervention threshold for several reasons. Firstly, the fracture risk varies markedly in different countries, but the T-score varies only by a small amount. Secondly, the significance of any given T-score to fracture risk in women from any one country depends on age (see Fig. 1) and the presence of clinical risk factors. Intervention thresholds will also be determined in part by the cost and benefits of treatment. In addition, since the T-score for BMD decreases with age, a T-score of, say, − 2.5 SD becomes less significant as a risk indicator with age [118,119,120]. Thus, with advancing age, the difference in the probability of fracture between the general population and those with a T-score of − 2.5 SD diminishes and indeed, from the age of 78 years in the USA and 81 years onwards in Kuwait, the fracture probability becomes progressively lower than that of the age and sex-matched individuals (Fig. 5). In other words, a T-score of − 2.5 SD becomes a diminishing risk factor with advancing age. In contrast, a prior fragility fracture is a highly significant risk factor at all ages (see Fig. 5).
Ten-year probabilities (%) of a major osteoporotic fracture for women from Kuwait at a T-score of − 2.5 SD (open triangle), − 1.5 SD (open square) and prior fracture (open diamond). The shaded area represents fracture probabilities in women with no clinical risk factors and average BMD. From [120] with kind permission from Springer Science and Business Media
The use of FRAX in clinical practice demands a consideration of the fracture probability at which to intervene, both for treatment (an intervention threshold) and for BMD testing (assessment thresholds). Many approaches have been used to set intervention thresholds with FRAX [89]. The thresholds used have varied since they depend critically on local factors such as reimbursement issues, health economic assessment, willingness to pay for health care in osteoporosis and access to DXA. For this reason, it is not possible or desirable to recommend a unified intervention strategy. The strategy given below draws on that most commonly applied in Europe in the context of postmenopausal osteoporosis but takes account that access to DXA varies markedly in different European countries [117].
Since many guidelines recommend that women with a prior fragility fracture may be considered for intervention without the necessity for a BMD test (other than to monitor treatment), a prior fracture can be considered to carry a sufficient risk that treatment can be recommended. For this reason, the intervention threshold in women without a prior fracture can be set at the age-specific fracture probability equivalent to women with a prior fragility fracture [114] and therefore rises with age, for example, from a 10-year probability of 8 to 33% in the UK [121]. In other words, the intervention threshold is set at the ‘fracture threshold’. This is the approach to intervention thresholds proposed or used in Belgium, Finland, France, Italy, Ireland, Poland, Romania, Russia, Spain, Switzerland and by the National Osteoporosis Guideline Group (NOGG) in the UK [89, 122] and European guidelines for glucocorticoid-induced osteoporosis [123]. Incidentally, the same intervention threshold is applied to men, since the effectiveness and cost-effectiveness of intervention in men is broadly similar to that in women for equivalent risk [42, 121, 124]. The approach used has been well validated and the intervention strategy shown to be cost-effective [114, 125,126,127,128].
Using this criterion, the intervention threshold will vary from country to country because the population risks (of fracture and death) vary [91, 129]. The fracture probability in women with a prior fracture in the five major EU countries is shown in Fig. 6. Probabilities are highest in the UK and lowest in Spain. The difference between countries is most evident at younger ages and becomes progressively less with advancing age.
The 10-year probability of a major osteoporotic fracture by age in women with a prior fracture and no other clinical risk factors in the five major EU countries as determined with FRAX (version 3.5). Body mass index set to 24 kg/m2 without BMD. From [3], with kind permission from Springer Science and Business Media
For the purposes of illustration in this guidance, an aggregate value is chosen. Thus, for the countries shown in Fig. 6, the mean probability of a major fracture in women with a prior fracture is 6.3% between the ages of 50 and 55 years. The mean is weighted for population size in each age interval in each country. The probability rises with age (Table 6) and can be taken as an intervention threshold. Countries with much higher or lower probabilities may wish to develop intervention thresholds based on country-specific risks as has been adopted in several countries in Europe and elsewhere. Note that the example in Table 6 uses the probability of a major osteoporotic fracture to determine an intervention threshold fracture. In addition to the 10-year probability of a major osteoporotic fracture, intervention thresholds can be based on the 10-year probability of hip fracture. Either or both thresholds can be used as recommended in the recent NOGG guidance [85].
Assessment thresholds for BMD testing
The assessment strategy outlined in Fig. 4 requires the determination of assessment thresholds for making recommendations for the measurement of BMD. There are, in principle, two assessment thresholds [114]:
A threshold probability below which neither treatment nor a BMD test should be considered (lower assessment threshold).
A threshold probability above which treatment may be recommended irrespective of BMD (upper assessment threshold).
Most countries adopt a case-finding strategy where individuals with clinical risk factors are identified for further assessment [12]. For this scenario, the lower assessment threshold can be set to exclude a requirement for BMD testing in women without clinical risk factors, as given in previous European guidelines [1,2,3, 123]. The probability equivalents are given in Table 6. In a few countries, population-based assessment with BMD is recommended (Germany and France in Europe). In such cases, there would be no lower assessment threshold.
An upper threshold can be chosen to minimise the probability that a patient characterised to be at high risk on the basis of clinical risk factors alone would be reclassified to be at low risk with additional information on BMD [125]. In the UK, the upper assessment threshold was set at 1.2 times the intervention threshold [114]. The rationale is that reclassification of risk with the addition of a BMD test (from high risk to low risk and vice versa) is high when fracture probabilities estimated without BMD are close to the intervention threshold and the likelihood of reclassification decreases the further away the probability estimate is from the intervention threshold [125]. When patients have a fracture probability that is 20% or more than the intervention threshold, almost no individuals will be reclassified (from high to low risk) when probabilities are recomputed with the addition of BMD to FRAX [124, 130,131,132]. Thus, a quotient of 1.2 is applied to the intervention, illustrated for the European example in Table 6. An attraction of the approach is that efficient use is made of BMD testing.
Application of probability thresholds
The application of these assessment thresholds depends critically on the availability (and reimbursement) of densitometry, which vary from country to country. It has been estimated that the requirements to service osteoporosis amount to approximately 11 DXA units/millions of the general population [117], though this estimate probably requires updating to take account of population demography. The availability of DXA falls above this estimate in a minority of European countries (Fig. 7). The large variation in resources for BMD testing demand the consideration of three assessment scenarios that depend on the access to central densitometry.
Unrestricted access to densitometry
Where resources for BMD testing are adequate, BMD tests can be undertaken in women with any clinical risk factors as shown in Fig. 8. Treatment is recommended where fracture probability exceeds the intervention threshold. Note that the lower assessment threshold is set as equivalent to women without clinical risk factors (see above). In those countries where screening of women without risk factors is recommended, there would be no lower assessment threshold. An additional option is to recommend treatment in women with a prior fragility fracture without recourse to BMD (though BMD might be undertaken to monitor treatment).
Assessment of major osteoporotic fracture risk in countries with high access to DXA. DXA is undertaken in women with a clinical risk factor. Assessment with DXA and/or treatment is not recommended where the FRAX probability is lower than the lower assessment threshold (green area). BMD is recommended in other women and treatment recommended where the fracture probability exceeds the intervention threshold (dotted line). The intervention threshold used is that derived from Table 6. From [3], with kind permission from Springer Science and Business Media
The assessment algorithm is summarised in Box 1. BMD tests are recommended in all postmenopausal women with a clinical risk factor.
Limited access to densitometry
Several countries must take a parsimonious approach to the use of BMD. The guidance recommends that postmenopausal women with a prior fragility fracture may be considered for intervention without the necessity for a BMD test. In women without a fragility fracture but with one or more other CRF, the intervention threshold is set at the age-specific fracture probability equivalent to women with a prior fragility fracture and BMD testing recommended in those in whom fracture probability lies between the upper and lower assessment threshold as described above [114] This approach, adapted to the common EU thresholds shown in Table 6, is illustrated in Fig. 9.
Assessment guidelines based on the 10-year probability of a major osteoporotic fracture (%). The dotted line denotes the intervention threshold. Where assessment is made in the absence of BMD, a BMD test is recommended for individuals where the probability assessment lies in the orange region. The intervention threshold and BMD assessment thresholds used are those derived from Table 6. From [3], with kind permission from Springer Science and Business Media
The assessment algorithm is summarised in Box 2.
No access or patchy access to densitometry
In countries with very limited or no access to DXA, FRAX can be used without BMD. For the purpose of risk assessment, a characteristic of major importance is the ability of a technique to predict fractures, traditionally expressed as the increase in relative risk per standard deviation (SD) unit decrease in risk score—termed the gradient of risk. The gradient of risk with FRAX is shown in Table 7 for the use of the clinical risk factors alone, femoral neck BMD and the combination [90].
The use of clinical risk factors alone provides a GR that lies between 1.4 and 2.1, depending upon age and the type of fracture predicted. These gradients are comparable to the use of BMD alone to predict fractures [32, 41]. For example, for the prediction of any osteoporotic fracture, the GR at the age of 70 years was 1.5 with femoral neck BMD [32]. With peripheral BMD, the gradient of risk is somewhat, though not significantly lower (GR = 1.4/SD; 95% CI = 1.3–1.5/SD). These data suggest that clinical risk factors alone are of value and can be used, therefore, in the many countries where DXA facilities are insufficient (Box 3). The rationale for the use of FRAX in the absence of access to BMD or limited access has been recently reviewed [65, 89]. Briefly, most of the risk factors incorporated within FRAX contribute independently from BMD to fracture risk, but are not totally independent of BMD; thus, higher risk is associated with lower underlying BMD [125, 132].
In several countries (Finland, Lebanon, Romania, UK), there is a link between the FRAX web site to an independent site that plots the FRAX output against the intervention thresholds for that country and facilitates treatment decisions. The NOGG web site in the UK is widely used (https://www.sheffield.ac.uk/NOGG/) [133].
Alternative approaches to intervention thresholds
The NOGG guidelines in the UK have recently been revised [134]. The intervention threshold up to age 70 years is set at a risk equivalent to that associated with a prior fracture, in line with current clinical practice, and therefore rises with age. At age 70 years and above, however, a fixed threshold is applied [134]. The alternative thresholds equilibrate fracture risk, particularly hip fracture risk, in those with or without prior fracture selected for treatment and reduce BMD usage at older ages. This modification from the age of 70 years is not necessarily applicable to other countries and would require the impact of changes to be evaluated.
An alternative approach to intervention thresholds has been applied in Germany, which uses a country-specific algorithm to estimate the 10-year incidence (not probability) of fracture [135].
Several guidelines in Europe that use FRAX have recommended that a fixed probability threshold be used as an intervention threshold. Examples include a 20% 10-year probability of a major fracture in several European countries and a 15% probability in Sweden [89]. Many utilise a threshold probability of 20% for a major osteoporotic fracture many of which also mention a hip fracture probability of 3% as an alternative intervention threshold. In nearly all instances, no rationale is provided other than the fact that this was the threshold used by the National Osteoporosis Foundation of the USA [116]. The rationale for a fixed threshold in the USA was based on the fracture probability at which intervention becomes cost-effective in the USA and is, therefore, not relevant for any other country.
The impact of using a fixed intervention threshold is shown in Fig. 10 for postmenopausal women in the UK. At high thresholds e.g. > 20% fracture probability 17% of postmenopausal women would be eligible for treatment. A problem that arises is that very few women under the age of 60 years would ever attain this threshold. On the other hand, if a less stringent threshold were chosen, say 5%, then nearly all women at the age of 50 years and above would exceed this threshold. Both scenarios could be justified on health economic criteria in the UK [128], but both are counterintuitive to clinical practice. Critically, economic criteria should not be used to set intervention thresholds but, more appropriately, to validate the implementation of clinically driven intervention thresholds [136].
The impact of a fixed treatment threshold in postmenopausal women in the UK according to threshold values for the probability of a major osteoporotic fracture. The left-hand panel shows the proportion of the postmenopausal population exceeding the threshold shown at each age. The right-hand panel shows the proportion of the total postmenopausal population that exceed a given threshold. From [3], with kind permission from Springer Science and Business Media
Other assessment models
As well as the FRAX tool, other fracture risk calculators are available online which include the Garvan fracture risk calculator and QFracture® [69, 70]. A fundamental difference between these risk models and FRAX is that the parameters of risk differ (incidence vs. probabilities) so that comparative data are not readily interpreted [137] (Fig. 11). In FRAX, fracture probability is computed taking both the risk of fracture and the risk of death into account. This is important because some of the risk factors affect the risk of death as well as the fracture risk. Examples include increasing age, sex, low BMI, low BMD, use of glucocorticoids and smoking.
The risk of hip fracture with age in a model that considers 10-year fracture risk alone (the Garvan tool) and FRAX, which computes the probability of hip fracture from the fracture and death hazards (FRAX). The T-scores are set differently in the two models so that the risks are approximately equal at the age of 60 years. Data are computed from the respective web sites [137]. With kind permission from Springer Science and Business Media
Effectiveness of risk assessment strategies
Until recently, the effectiveness of risk-assessment strategies in which samples of the general population might be evaluated for risk factors and BMD estimation to derive individual estimates of absolute fracture risk, with targeting of anti-osteoporosis therapy on the basis of these estimates, remained uncertain. The publication of the MRC SCOOP trial (SCreening of Older wOmen for the Prevention of fractures) provides strong support for such a strategy [111]. This seven-centre pragmatic randomised controlled trial with 5-year follow-up included 11,580 women aged 70–85 years, who were randomised to receive a care algorithm including FRAX and drug targeting (n = 6233) or usual primary care for osteoporosis based on opportunistic case finding (n = 6250). Women were recruited from 100 UK general practices, and the principle outcome measures were major osteoporotic, hip and all fractures. Screening reduced the incidence of hip fractures (0.72, 0.59–0.89, p = 0.002). The effect on hip fracture increased significantly with baseline FRAX hip fracture probability (p = 0.021 for interaction); for example, at the 10th percentile of baseline FRAX hip probability (2.6%), hip fractures were not significantly reduced (HR 0.93, 0.71 to 1.23), but at the 90th percentile (16.6%), there was a 33% reduction (HR 0.67, 0.53 to 0.84) [112]. The screening algorithm resulted in a pronounced increase in the use of anti-osteoporosis medication, and greater compliance with therapy, over the period of follow-up. These findings strongly support a systematic, community-based screening programme of fracture risk in older women. In addition, the strategy appears to be cost-effective [138].
General management
Mobility and falls
Immobilisation causes of bone loss. Immobilised patients when confined to bed may lose as much bone in a week than they would otherwise lose in a year. Weight-bearing exercise forms an integral component of osteoporosis management [139,140,141]. The amount of weight-bearing exercise that is optimal for skeletal health in patients with osteoporosis is not known. Physiotherapy is an important component of rehabilitation after fracture. At all times, exercises to improve muscle strength and balance may prevent falls by restoring confidence and coordination, and additionally maintain bone mass by stimulating bone formation and decreasing bone resorption.
Such measures can be coupled with a programme to reduce the likelihood of falls in those at high risk [142, 143]. Modifiable factors such as correcting decreased visual acuity, reducing consumption of medication that alters alertness and balance, and improving the home environment (slippery floors, obstacles, insufficient lighting, handrails) are important measures aimed at preventing falls [144]. Fall prevention exercise interventions have been shown to reduce the risk of injurious falls and of fracture [145]. Whole body vibration may be beneficial for falls risk reduction, but without effect on BMD or fracture risk [146]. Some randomised trials have shown that wearing hip protectors can reduce hip fracture risk, particularly in the elderly living in nursing homes. A meta-analysis of well-conducted randomised controlled trials has, however, cast some doubt about the anti-fracture efficacy of this preventive measure [147,148,149,150].
Nutrition
At every stage of life, adequate dietary intakes of key bone nutrients such as calcium, vitamin D and protein contribute to bone health and reduce thereby the risk of osteoporosis and of fracture later in life [151]. Dietary sources of calcium are the preferred option and calcium supplementation should only be targeted to those who do not get sufficient calcium from their diet and who are at high risk for osteoporosis. The Recommended Nutrient Intakes are 800–1000 mg of calcium and 800 IU of vitamin D per day in men and women over the age of 50 years [152].
Combined calcium and vitamin D supplements in a daily dose of 0.5–1.2 g and 400–800 IU, respectively, are generally recommended in patients receiving bone protective therapy, since most randomised controlled trial evidence for the efficacy of interventions is based on co-administration of the agent with calcium and vitamin D supplements [153]. Calcium and vitamin D supplements may decrease secondary hyperparathyroidism and reduce the risk of proximal femur fracture, particularly in the elderly living in nursing homes [154, 155]. In six trials included in the meta-analysis [155], hip fracture risk was 0.61 (95% CI 0.46–0.62) with calcium and vitamin D supplementation. In contrast, a recent meta-analysis did not find a reduction in fracture risk in community-dwelling older adults receiving calcium, vitamin D, or the combination [156]. The latter included seven trials, but only three among those analysed in [155]. Adding to the controversies over calcium, a meta-analysis has concluded that calcium supplements without co-administered vitamin D were associated with an increase in the risk of myocardial infarction by around 30% [157]. Cardiovascular outcomes were not primary endpoints in any of the studies and the association remains the subject of some controversy [158,159,160,161,162,163].
Overall, it can be concluded that (1) calcium and vitamin D supplementation may lead to a modest reduction in fracture risk, although population-level intervention has not been shown to be an effective public health strategy; (2) supplementation with calcium alone does not reduce fracture risk; (3) side effects of calcium supplementation include renal stones and gastrointestinal symptoms; (4) vitamin D supplementation, rather than calcium, may reduce falls risk; and (5) increased cardiovascular risk consequent to calcium supplementation is not convincingly supported by current evidence; (6) calcium and vitamin D supplementation is recommended for patients at high risk of calcium and vitamin D insufficiency, and in those who are receiving treatment for osteoporosis [153]. This approach appears to be cost-effective [164].
Vitamin D supplements alone may reduce the risk of fracture and falls provided the daily dose of vitamin D is greater than 700 IU [165, 166]. In contrast, studies with large annual doses of vitamin D have reported an increased risk of hip fracture and, in one study, and also of falls [167, 168]. The upper limit of vitamin D dose that is beneficial on falls may be lower than previously estimated [169, 170].
Whereas a gradual decline in caloric intake with age can be considered as an appropriate adjustment to the progressive reduction in energy expenditure, a parallel reduction in protein intake may be detrimental for maintaining the integrity and function of several organs or systems, including skeletal muscle and bone. Sufficient protein intakes are necessary to maintain the function of the musculoskeletal system, but they also decrease the complications that occur after an osteoporotic fracture [151, 171]. Correction of poor protein nutrition in patients with a recent hip fracture has been shown to improve the subsequent clinical course by significantly lowering the rate of complications, such as bedsores, severe anaemia and intercurrent lung or renal infection. The duration of hospital stay of elderly patients with hip can thus be shortened [151].
Dairy products are a source of both protein and calcium, since 1 L of milk provides 32 g of protein and 1200 mg of calcium. Dairy products, some being fortified with calcium or vitamin D, decrease circulating PTH, increase IGF-I and decrease bone resorption markers [171,172,173]. Dairy products are associated with higher bone strength in both men and women [174, 175]. In older US men and women, higher milk consumption is associated with a lower hip fracture risk [176]. Fermented milk products like yogurt or soft cheese may provide larger amounts of these nutrients than the same volume of plain milk because of enrichment with milk powder to make the yogurt matrix denser [177,178,179]. Thus, calcium and vitamin D fortified dairy products (yogurt, milk) providing at least 40% of the RNI of calcium (400 mg) and 200 IU of vitamin D per portion are valuable options for covering the needs in the oldest old. Cheese consumption is associated with lower mortality [180]. Several studies have concluded to a favourable cost-effectiveness of dairy products in osteoporosis management [181,182,183,184].
Major pharmacological interventions
The most commonly used agents in Europe are raloxifene, the bisphosphonates alendronate, ibandronate, risedronate and zoledronic acid, agents derived from parathyroid hormone and denosumab. They have all been shown to reduce the risk of vertebral fracture. Some have also been shown to reduce the risk of non-vertebral fractures and, in some cases, agents have been shown specifically to decrease fracture risk at the hip (Table 8) [3, 85, 185, 186].
Selective oestrogen receptor modulators
Selective oestrogen receptor modulators (SERMs) are nonsteroidal agents that bind to the oestrogen receptor and act as oestrogen agonists or antagonists, depending on the target tissue. The concept of SERMs was triggered by the observation that tamoxifen, which is an oestrogen antagonist in breast tissue, is a partial agonist on bone, reducing the rate of bone loss in postmenopausal women [187]. Raloxifene is the only SERM widely available for the prevention and treatment of postmenopausal osteoporosis, but several others are in clinical development. Raloxifene prevents bone loss [188] and reduces the risk of vertebral fractures by 30–50% in postmenopausal women with low bone mass, and with osteoporosis with or without prior vertebral fractures as shown in the MORE trial [188]. There was no significant reduction of non-vertebral fractures. In women with severe vertebral fractures at baseline (i.e. at highest risk of subsequent fractures), a post hoc analysis showed a significant reduction of non-vertebral fractures [189].
In the MORE study and its placebo-controlled 4-year follow-up (CORE), the only severe (but rare) adverse event was an increase of deep venous thromboembolism. Hot flushes and lower limb cramps are commonly reported. There was a significant and sustained decrease of the risk of invasive breast cancer (by about 60%) [190], that has been subsequently confirmed in two other large cohorts, including the STAR study that showed similar breast cancer incidences with raloxifene and tamoxifen in high-risk populations [191]. The RUTH study, performed in postmenopausal women at high risk of cardiovascular disease [192], showed that raloxifene had no effect on cardiovascular death, and on the incidence of coronary heart disease and stroke [193]. However, an increased risk of death from stroke has been reported in women with or at risk of coronary heart disease. The efficacy of raloxifene has been shown in women with osteopenia [194] and is not dependent on the level of fracture risk assessed by FRAX [195]. In summary, the overall risk-benefit ratio of raloxifene is favourable and the drug is approved widely for the prevention and treatment of postmenopausal osteoporosis.
Bazedoxifene is a selective oestrogen receptor modulator that has been approved in Europe but is only available in Spain and Germany. In phase 3 clinical trials, bazedoxifene was shown to reduce the risk of new vertebral fracture, with favourable effects on bone mineral density, bone turnover markers and the lipid profile [196, 197]. The phase III study was extended up to 7 years [198]. During this period, the efficacy and safety of bazedoxifene were sustained. Two separate network meta-analyses provided an indirect comparison of the effect of bazedoxifene versus oral bisphosphonates, for the prevention of vertebral [199] and non-vertebral fractures [200], respectively. They concluded that bazedoxifene is expected to have at least a comparable relative risk reduction of vertebral [199] and non-vertebral fracture [200] as alendronate, ibandronate and risedronate. In a post hoc study in a subgroup of women at increased risk of fracture, bazedoxifene decreased non-vertebral fracture risk. In contrast to raloxifene, the efficacy of bazedoxifene is dependent on the level of fracture risk assessed by FRAX [201]. In common with raloxifene, venous thromboembolic events, primarily deep vein thromboses, leg cramps and hot flushes were more frequently reported in the active treatment groups compared with the placebo group [202].
Bazedoxifene has been combined with conjugated equine oestrogen to create a tissue selective oestrogen complex for the management of vasomotor symptoms and the prevention of osteoporosis associated with menopause [203]. A series of five phase III studies known as the Selective estrogen, Menopause And Response to Therapy (SMART) trials led to the approval, by the US Food and Drug Administration (FDA) and in Europe, of a daily dose of bazedoxifene 20 mg/conjugated equine oestrogen 0.45 mg. This association improved vasomotor symptoms whilst opposing breast and endometrial proliferation, preventing bone resorption and improving lipid profiles [203]. Over 12 months, this combination product improved BMD at the spine and at the hip, reduced markers of bone turnover and significantly improved vasomotor function score in a population of European postmenopausal women without effects on fracture risk [204].
Bisphosphonates
Bisphosphonates are stable analogues of pyrophosphate characterised by a P-C-P bond. A variety of bisphosphonates has been synthesised, the potency of which depends on the length and structure of the side chain [205]. Bisphosphonates have a strong affinity for bone apatite, both in vitro and in vivo, which is the basis for their clinical use. They are potent inhibitors of bone resorption and produce their effect by reducing the recruitment and activity of osteoclasts and increasing their apoptosis. The potency and chemical affinity to bone of bisphosphonates determines their effect to inhibit bone resorption and varies greatly from compound to compound. Potency differences can range 10,000-fold in vitro, so that the doses used clinically also vary. The mechanism of action on osteoclasts includes inhibition of the proton vacuolar adenosine triphosphatase (ATPase) and alteration of the cytoskeleton and the ruffled border. Amino-bisphosphonates also inhibit the farnesyl pyrophosphate synthase step in the mevalonate pathway, thereby modifying the isoprenylation of guanosine triphosphate binding proteins.
Oral bioavailability of bisphosphonates is low, around 1% of the dose ingested, and is impaired by food, calcium, iron, coffee, tea and orange juice. Bisphosphonates are quickly cleared from plasma, about 50% being deposited in bone and the remainder excreted in urine. Their half-life in bone is very prolonged [206].
Alendronate 70 mg once weekly and risedronate 35 mg once weekly are the most commonly used bisphosphonates worldwide. In the Fracture Intervention (FIT) study, alendronate was shown to reduce the incidence of vertebral, wrist and hip fractures by approximately half in women with prevalent vertebral fractures [207,208,209]. In women without prevalent vertebral fractures, there was no significant decrease in clinical fractures in the overall population, but the reduction was significant in the one third of patients that had a baseline hip BMD T-score lower than − 2.5 SD [210]. In a population of more than 90,000 men and women aged 80 years and older and who had sustained a prior fracture, a case-control analysis revealed that alendronate use was associated with a 34% decrease in hip fracture risk, and a 12% lower mortality risk but with a 58% increase in the risk of mild upper gastrointestinal symptoms [211].
Risedronate has been shown to reduce the incidence of vertebral and non-vertebral fractures by 40–50% and 30–36%, respectively, in women with prevalent vertebral fractures [212, 213]. In a large population of elderly women, risedronate decreased significantly the risk of hip fractures by 30%, an effect that was greater in osteoporotic women age 70–79 years (− 40%), and not significant in women over the age of 80 years without evidence of osteoporosis [71]. A delayed-release formulation of 35 mg risedronate weekly, given before or immediately following breakfast, showed a similar or greater effect on spine and hip BMD than traditional immediate-release 5 mg risedronate daily. This formulation allows osteoporotic patients to take their weekly risedronate dose immediately after breakfast, hence offering a potential for improved adherence and persistence to treatment [214].
Ibandronate given daily (2.5 mg) reduces the risk of vertebral fractures by 50–60%. An effect on non-vertebral fractures was only demonstrated in a post hoc analysis of women with a baseline of BMD T-score below − 3 SD [215,216,217]. Bridging studies have shown that oral ibandronate 150 mg once monthly is equivalent or superior to daily ibandronate in increasing BMD and decreasing biochemical markers of bone turnover, giving rise to its approval for the prevention of vertebral fracture in postmenopausal osteoporosis [218]. The efficacy and safety of oral monthly ibandronate was confirmed for up to 5 years in women with postmenopausal osteoporosis [218, 219]. Similarly, bridging studies comparing intermittent intravenous ibandronate to daily oral treatment has led to the approval of intravenous ibandronate 3 mg every 3 months for the same indication [220]. A post hoc analysis of pooled individual patient data from the studies assessing the long-term (5 years) efficacy of oral [218] and intravenous [221] ibandronate concluded that for ibandronate regimens with annual cumulative exposure ≥ 10.8 mg, time-to-fracture was significantly longer for all clinical fractures, non-vertebral and clinical vertebral fractures versus placebo and that for all fracture types, the rate of fracture appeared stable up to 5 years [222].
Based on the result of a phase II study [223], a large phase III trial in over 7700 postmenopausal osteoporotic patients assessed the efficacy of yearly infusion of zoledronic acid 5 mg over 3 years. As compared to the placebo group, zoledronic acid was found to reduce the incidence of vertebral fractures by 70% and that of hip fractures by 40% [224] and is now available for the treatment of postmenopausal osteoporosis. Intravenous zoledronic acid has also been shown to decrease the risk of fracture and mortality when given shortly after a first hip fracture [225]. The phase III trial was extended to 6 [226] and 9 [227] years. The overall conclusion was that pursuing treatment beyond 3 years only provided marginal benefits [227]. Some authors even argue that an annual administration of 5 mg zoledronic acid might represent over treatment [228]. A single dose of 5 mg zoledronic acid given to frail elderly women improved spine and total hip BMD over 2 years, compared to placebo but the treated group had an increase in fractures, multiple falls and mortality [229] suggesting that zoledronic acid may not be an appropriate treatment for such patients.
Safety of bisphosphonates
The overall safety profile of bisphosphonates is favourable. Oral bisphosphonates are associated with mild gastrointestinal disturbances, and some amino-bisphosphonates (alendronate and pamidronate) can rarely cause oesophagitis. A network meta-analysis compared the gastrointestinal safety of all oral and injectable bisphosphonates given to osteoporotic patients. It concluded that zoledronic acid has the highest probability of causing gastrointestinal adverse events, possibly related to nausea [230]. Intravenous amino-bisphosphonates can induce a transient acute phase reaction with fever, bone and muscle pain that ameliorates or disappears after subsequent courses [231].
Osteonecrosis of the jaw has been described in cancer patients receiving high doses of intravenous pamidronate or zoledronate. The incidence in osteoporotic patients treated with oral and intravenous bisphosphonates appears to be very rare (in the order of 1/100,000 patient-year), only slightly higher than the incidence in the general population [232, 233]. The risk of osteonecrosis of the jaw is reported to be greater with a longer duration of bisphosphonate therapy [234, 235], but this finding is not consistent [232]. Possible explanations relate to the class of bisphosphonate, differences in potency and route of administration. The time to onset of osteonecrosis of the jaw may be shorter for intravenous zoledronic acid compared to oral alendronate [236] [237].
Concerns have been raised about a possible association between bisphosphonate therapy and atrial fibrillation. Subsequent studies have produced conflicting results, but have not excluded the possibility of such an association in people at increased risk of fracture [238]. Patients to whom zoledronic acid was administered for up to 9 years had a higher risk of cardiac arrhythmias compared to those who discontinued the treatment after 6 years [227].
The possibility that bisphosphonate therapy is associated with increased risk of oesophageal cancer has been raised. Two studies from the General Practice Research Database in the UK have produced conflicting results, one failing to show any association but another concluding that there was an increased risk with extended use over 5 years [239, 240]. Finally, bisphosphonate use may be associated with atypical subtrochanteric fractures [241,242,243]. Likewise, associations between bisphosphonate exposure and lower risks of mortality and cancer also require further scrutiny [244,245,246,247]. The risk-benefit ratio remains favourable for the use of bisphosphonates to prevent fractures [242].
Many authors recommend that patients be reviewed after 3 years (IV) or 5 years (oral) treatment with bisphosphonate [85, 232, 235, 237]. It is appropriate that periodic assessment of fracture risk should use FRAX with femoral neck BMD [85]. Fracture risk should be reassessed after a new fracture, regardless of when it occurs [85]. Although some advocate a ‘drug holiday’, prospective and retrospective analyses report that the risk of new clinical fractures was 20–40% higher in subjects who stopped treatment [248, 249] and vertebral fracture risk was approximately doubled [226, 250].
A substantial body of evidence indicates that some generic formulations of alendronate are more poorly tolerated than the proprietary preparations, which results in significantly poorer adherence and thus effectiveness [251].
Peptides of the parathyroid hormone family
The continuous endogenous production of parathyroid hormone (PTH), as seen in primary or secondary hyperparathyroidism, or its exogenous administration can lead to deleterious consequences for the skeleton, particularly on cortical bone. However, intermittent administration of PTH (e.g. with daily subcutaneous injections) results in an increase of the number and activity of osteoblasts, leading to an increase in bone mass and in an improvement in skeletal architecture at both cancellous and cortical skeletal sites [252].
The 1-34 N-terminal fragment (teriparatide) is used for the management of osteoporosis. The marketing authorisation for the 1 to 84 intact molecule has been withdrawn at the request of the marketing authorisation holder. Treatment with teriparatide has been shown to reduce significantly the risk of vertebral fractures and also non-vertebral fractures. There is no convincing evidence that teriparatide reduces hip fracture, but this may reflect absence of evidence, not evidence of absence. Thus, the recommendation for its use in high-risk people is particularly strong in patients with vertebral fracture. The recommended dose is 20 μg of teriparatide, given as a subcutaneous injection [253]. Treatment with PTH has been studied when given for 18 to 24 months and beneficial effects on non-vertebral fracture with teriparatide have been shown to persist for up to 30 months after stopping teriparatide [254].
The most common reported adverse events in patients treated with PTH or teriparatide are nausea, pain in the limbs, headache and dizziness. In normocalcaemic patients, slight and transient elevations of serum calcium concentrations have been observed following the injection teriparatide. Serum calcium concentrations reach a maximum between 4 and 6 h and return to baseline 16 to 24 h after each dose. The change is small and routine monitoring of serum calcium during therapy is not required. PTH and teriparatide may cause small increases in urine calcium excretion but the incidence of hypercalciuria does not differ from that in placebo-treated patients. However, these agents should be used with caution in patients with active or recent urolithiasis because of their potential to exacerbate the disorder. Isolated episodes of transient orthostatic hypotension are also reported. They typically resolve within minutes to a few hours, and do not preclude continued treatment.
The use of peptides of the PTH family is contraindicated in conditions characterised by abnormally increased bone turnover (e.g. pre-existing hypercalcaemia, metabolic bone diseases other than primary osteoporosis, including hyperparathyroidism and Paget’s disease of bone, unexplained elevation of alkaline phosphatase, prior external beam or implant radiation therapy to the skeleton or in patients with malignancies or bone metastasis). Severe renal impairment is also a contraindication. Studies in rats have indicated an increased incidence of osteosarcoma, with long-term administration of very high doses of teriparatide [255, 256]. These findings have not been considered relevant for patients treated with very much smaller doses of teriparatide.
Denosumab
Critical molecules for the differentiation, activation and survival of osteoclasts are the receptor activator of nuclear factor NFkB (RANK), its ligand RANKL, a member of the tumour necrosis factor (TNF) superfamily, and osteoprotegerin (OPG), which acts as a decoy receptor for RANKL. A fully human antibody against RANKL has been developed. This antibody, denosumab, has been shown to specifically bind to RANKL with a very high affinity, preventing its interaction with the receptor RANK [257].
The anti-fracture efficacy of 60 mg denosumab given subcutaneously every 6 months has been evaluated in postmenopausal osteoporotic women. After 3 years, there was a 68% reduction in the incidence of new vertebral fractures. The incidence of clinical vertebral fractures was similarly reduced by 69%. The incidence of non-vertebral fractures was reduced by 20% and of hip fractures by 40% [258]. After completing the first 3 years of the study, women from the denosumab group had 7 more years of denosumab treatment (long-term group) and those from the placebo group had 7 years of denosumab exposure (cross-over group) [259]. The yearly incidence of new vertebral fractures remained low during the extension, whereas non-vertebral fractures further significantly decreased in year 4 [260] and thereafter remained stable (approximately 1.5% per year for both vertebral and non-vertebral fractures) [235, 259]. The incidence of vertebral and non-vertebral fracture observed during the extension was similar to that observed in the denosumab group during the first 3 years and lower than rates projected from a virtual long-term placebo cohort [259].
Discontinuation of denosumab is associated with a rapid offset of action: Markers of bone turnover increased to above baseline levels, which returned to baseline values within 1 to 2 years after stopping treatment [261] and BMD decreased to baseline values by 12–18 months, independently of the duration of treatment [261]. In a sample of 1000 patients who discontinued denosumab during the 3-year pivotal study [258] or its extension [259], the vertebral fracture rate increased to a value similar to that observed in participants who received and then discontinued placebo [262]. The proportion of patients developing multiple vertebral fractures after stopping treatment was higher in the denosumab group than in the placebo group. In addition, the odds of developing multiple vertebral fractures after stopping denosumab was increased in patients with prior vertebral fracture sustained before or during treatment, or in those with the longer exposure to denosumab [262]. No increase in non-vertebral fracture after denosumab cessation was reported. A short duration of bisphosphonate therapy could be considered when discontinuing denosumab to prevent the rebound effect [263]. In women transitioning from oral bisphosphonates to injectable treatments, denosumab was associated with greater BMD increases at all skeletal sites and greater inhibition of bone remodelling, compared with zoledronic acid [235, 264].
The incidence of adverse events for all individuals who received denosumab for 10 years [259] tended to decrease over time whereas serious adverse events were stable. One atypical femoral fracture occurred in each group during the extension. Seven cases of osteonecrosis of the jaw were reported in the long-term group and six cases in the cross-over group [259]. In a meta-analysis of four clinical trials, the relative risk of serious adverse events for the denosumab group compared with the placebo group was 1.33, of serious adverse events related to infection 2.10, of neoplasm 1.11, of study discontinuation due to adverse events 1.10, and of death 0.78. These risks were all non-significant [265].
Summary of effects
The effects of the major pharmacological interventions on vertebral and hip fracture risk are summarised in Table 9.
Combination and sequential treatments
These treatment regimens include the concomitant or sequential use of compounds sharing the same mode of action (e.g. two or more inhibitors of bone resorption) or agents with differing activities (e.g. an inhibitor of resorption plus an anabolic agent). None of the available studies has been powered so far, to assess differences in fracture incidence between combination therapy and monotherapy, but results obtained with BMD, bone histomorphometry, finite element analysis or markers of bone turnover shifted the treatment paradigm towards a greater use of combination or sequential therapies. Whereas the first attempts to combine alendronate and PTH were disappointing [266], combination of teriparatide and denosumab generated greater increments in BMD and calculated bone strength compared to either drug alone [267], supporting further investigation of this combination. Similarly, in alendronate-treated women, 3-month teriparatide cycles followed by 3-month off improve BMD similarly to daily continuous treatment with teriparatide, an observation which was not confirmed in alendronate-naive women [268]. In a controlled comparison of women who switched from alendronate to teriparatide versus those who added teriparatide to ongoing alendronate, the effect on hip BMD and on hip strength was greater with combination therapy. Continuing a potent anti-resorptive agent when starting a bone-forming agent might thus improve hip outcomes [269].
In patients at high risk of fracture, starting treatment with an anabolic agent seems most appropriate to promptly reduce the fracture risk [186]. Given that treatments with anabolic agents are limited to 18–24 months and that efficacy will wane once treatment is stopped, the real potential of the anabolic treatments is whether their greater effect on BMD and fracture can be maintained with the inhibitors of bone turnover once treatment is stopped (Fig. 12) [270]. In the absence of a subsequent prescription of an anti-resorptive agent, the benefits obtained during treatment with teriparatide progressively disappear [271], whereas they are maintained when denosumab [267] is prescribed, as soon as possible after stopping the anabolic intervention.
Schematic diagram showing the effects of a bone-forming agent on the relative fracture risk reduction (RRR) compared with placebo. In scenario A, treatment with a bone-forming agent induces a marked effect on fracture risk over an 18 months exposure compared with placebo. On stopping the bone-forming agent, the effect on fracture wanes off over a similar time interval of 18 months. In scenario C, placebo group remains untreated, whereas the group treated with a bone-forming agent is transitioned to an inhibitor of bone turnover, which maintains the efficacy up to 4 years. In scenario B, both the treatment and the placebo groups are treated after the exposure with an inhibitor of bone turnover [270]. With kind permission from Springer Science and Business Media
Other pharmacological interventions
Menopausal hormone therapy
Oestrogens reduce the accelerated bone turnover induced by the menopause and prevent bone loss at all skeletal sites regardless of age and duration of therapy. Results from observational studies and randomised placebo-controlled trials have shown that estrogens decrease the risk of vertebral and non-vertebral fractures (including hip fracture) by about 30%, regardless of baseline BMD [272, 273]. When hormone replacement therapy is stopped, bone loss resumes at the same rate as after the menopause, but fracture protection may persist arguably for several years [274, 275].
The original analyses of the Women’s Health Initiative (WHI) suggested, however, that the long-term risks of menopausal hormone therapy (MHT) outweighed the benefits. In this large cohort of postmenopausal women in their 60s, the combined use of conjugated oestrogen and medroxyprogesterone acetate was originally associated with a 30% increased risk of coronary heart disease (CHD), and breast cancer and with a 40% increase in stroke [276,277,278]. There was also a slight increase in the risk of dementia [279], and no clinically meaningful effect on health-related quality of life such as sleep disturbance or vasomotor symptoms [280]. In a subsequent analysis, the increase in breast cancer risk was much less in women not previously exposed to MHT [278]. In hysterectomized women receiving conjugates oestrogen alone, there was also an increase in stroke, but not of CHD and breast cancer, suggesting a deleterious effect of medroxyprogesterone acetate [281]. It has been postulated that the benefits of HRT outweigh the risks in younger postmenopausal women [282, 283], but so far there is no placebo-controlled study showing the long-term safety of such approaches. However, in a recent publication, re-assessing the long-term outcomes of the WHI, MHT with conjugated oestrogen and medroxyprogesterone acetate for a median of 5.6 years or with conjugated oestrogen alone for a median of 7.2 years was not associated with an increased risk of all-cause, cardiovascular, or cancer mortality during a cumulative follow-up of 18 years [284]. This may challenge the current recommendation to use HRT only for climacteric symptoms, at a dose as small as possible and for a limited period of time [285].
Vitamin D derivatives
Alfacalcidol is a synthetic analogue of the vitamin D metabolite calcitriol (1,25-dihydroxyvitamin D3) and it is metabolised to calcitriol by its 25-hydroxylation in the liver. It is somewhat less potent than calcitriol. Both alfacalcidol and calcitriol are used in some countries for the treatment of osteoporosis. Several but not all studies show decreases in vertebral fracture risk [286, 287]. A meta-analysis suggested that combined treatment with alendronate and alfacalcidol prevented all osteoporotic fractures more than alfacalcidol or alendronate alone [288]. The effects on bone mineral density have been less extensively studied. A few reports have suggested that alfacalcidol and calcitriol exert a direct action on muscle strength and decreases the likelihood of falling in elderly subjects [289, 290].
The major problem with the use of the vitamin D derivatives is the risk of hypercalcaemia and hypercalciuria. Adverse effects of prolonged hypercalcaemia include impairment of renal function and nephrocalcinosis. The narrow therapeutic window demands the frequent surveillance of serum and possibly urine calcium in patients exposed to these agents. Calcium supplementation of the diet should be avoided or used with care.
Clodronate
Clodronate is a relatively weak bisphosphonate, but has been shown to decrease the risk of vertebral and non-vertebral fractures in randomised controlled studies [291, 292]. It is widely available for the treatment of neoplastic bone disease but licensed for use in osteoporosis in only a few countries.
Local osteo-enhancement procedure
Local osteo-enhancement procedure (LOEP) is a local treatment, which requires a minimally invasive injection in the femoral neck of a resorbable synthetic bone graft substitute, containing a proprietary triphasic calcium sulphate/calcium phosphate implant [293]. In postmenopausal women with low hip BMD (mean T-score = − 3.1), femoral neck BMD in treated hips increased by 58% compared to contralateral control hips, during 5–7 years of follow-up [293]. X-ray and QCT analyses demonstrated that the implant material was completely resorbed in all patients and replaced with bone that integrated with the surrounding trabecular and cortical bone [294]. QCT scans were used to conduct patient-specific, non-linear finite element analysis to estimate hip strength in simulated sideways fall and stance loading conditions. Femoral strength in sideway fall was 36% higher in treated than control femurs 5–7 years after the procedure [295]. No safety issues were reported during the study [293,294,295]. Data on fracture outcomes are not yet available.
Vertebroplasty and kyphoplasty
In patients with recent vertebral fracture in whom pain persists for 2 to 3 weeks despite a well-conducted analgesic programme, injection of cement in the fractured vertebral body without (vertebroplasty) or with preceding balloon inflation (kyphoplasty) may lead to reduction of pain and positive functional outcomes [296, 297]. Whether pain relief is related to the cement itself or to local anaesthetic is still unclear [298, 299]. Heterogeneity in treatment recommendations is, in part, explained by an insufficient clinical evidence base for vertebral augmentation and heterogeneity of patients, leading to undue reliance on expert opinion [300, 301]. An increase in new vertebral fracture rates at non-treated levels, especially those adjacent to the treated vertebrae, has been reported [297, 302] but not consistently [303] following both vertebroplasty and kyphoplasty.
Fracture liaison services
Fracture liaison services (FLS), also known as osteoporosis coordinator programmes and care manager programmes, provide a system for the routine assessment and management of postmenopausal women and older men who have sustained a fragility fracture [304,305,306]. Since the majority of patients presenting with fragility fracture do not receive appropriate assessment and treatment, fracture liaison services address this need through a systematic approach to identify cases, assess risk of further fractures and the need for treatment. Most fracture liaison services are based in secondary care although models in primary care have also been described. A dedicated coordinator, often a nurse, working closely with the patient, primary care physician, orthopaedic and trauma department and osteoporosis and falls service is central to the development of a successful service. An example of the structure of a fracture liaison service is shown in Fig. 13.
Schema of a Fracture Liaison Service (FLS) integrated with post-fracture falls risk assessment [after [307]]
The IOF has launched a global campaign (‘Capture the fracture®’) to promote this approach for the prevention of a second fracture [308, 309]. This initiative aims to set internationally endorsed standards for best practice by facilitating the implementation of fracture liaison services involving best practice frameworks, multidisciplinary models and FLS questionnaires.
The benefits of coordinator-based systems to ensure appropriate management of patients following a fracture are well established [7, 308,309,310,311,312,313,314,315]. Use of a systematic coordinator approach in the Kaiser Permanente Healthy Bones Program was associated with a 40% reduction in hip fractures [314]. Recent studies from the UK [316,317,318] reported that the initiation of FLS reduced the 30-day and 1-year mortality rates following hip fracture, led to a significant reduction in second fracture rate and increased the utilisation of anti-osteoporosis treatment by 15%. Although the health economic analyses that have been published so far have shown that osteoporosis management programmes are a cost-effective intervention for the prevention of fractures [314, 315, 319,320,321], larger and longer-term studies will be needed to further quantify the effect of FLS care on subsequent fracture risk [322].
Adherence and monitoring of treatment
Adherence to treatment
When discussing adherence, there is a need to define the terminology [323], since a wide variety of definitions is used in the literature.
-
1.
Adherence is a general term encompassing the aspects mentioned below.
-
2.
Persistence describes for how long the medication is taken. Persistence could be expressed as number of days until discontinuation or the proportion of the cohort still on the medication after a given time since first prescription. Non-persistence is assumed to be the same as discontinuation if a treatment gap is longer than a set number of days.
-
3.
Compliance denotes the proximity to the treatment recommendation as given in the official product information (SPC). It is often simplified to mean the number of doses taken divided by the number of prescribed doses. This simplification does not include some important aspects of compliance, such as taking medication with food (for the oral bisphosphonates), at the correct time of the day, too large doses to compensate for forgotten doses, pill dumping, etc.
-
4.
Primary non-adherence is when the patient is prescribed a drug and then never fills the prescription.
Non-adherence to medical therapy is a widespread public health problem. It is estimated that only half of the patients comply with long-term therapy of which a substantial minority do not even redeem their prescription. Overcoming non-adherence presents particular challenges in asymptomatic bone diseases and other chronic, asymptomatic conditions. In such settings, the level of perceived threat to health does not motivate the patient to adhere to therapy. In addition, risk of non-adherence with any therapy increases with increased duration of treatment [324].
Poor adherence to medication is associated with adverse effects on outcomes in osteoporosis or osteopenia, and non-adherent patients have smaller decreases in rates of bone turnover, smaller gains in BMD and a significantly greater risk of fracture [325,326,327]. Partial adherence also has a significant impact on cost-effectiveness [328]. Further research is required to optimise thresholds of compliance and persistence, the impact of gap length, offset times, and fraction of benefit [329].
Improving adherence to osteoporosis therapy requires effective patient/provider communication and close patient monitoring for the early identification of declining adherence. Patients’ belief in a medication contributes to better adherence and can be improved by firmly associating treatment with expected benefits such as reduced risk of fracture and thereby an improved quality of life. Patients may be encouraged to adhere when presented with measurements of biochemical markers of bone turnover or their BMD results together with an explanation of how these measures relate to risk reduction. Another primary component of improving adherence is to use simplified or user-friendly treatment programmes [330, 331]. Frequency of dosing is another determinant of adherence [332, 333]. A recent IOF and ECTS taskforce suggested that screening to detect a lack of adherence with oral bisphosphonates should involve the measurement of P1NP and CTX at baseline and 3 months after starting therapy. In the absence of a decrease above the least significant change (i.e. − 38% for P1NP and − 56% for CTX), a low adherence should be suspected [334].
It should be noted that inadequate adherence can also take the form of improper drug administration, even when doses are not missed. An example is the malabsorption of oral bisphosphonates when taken with food. Such non-adherence poses the potential problems of decreased drug absorption and increased risk of adverse effects [335].
Monitoring of treatment with densitometry
The goal of bone-targeted drug therapy in a patient with osteoporosis is to increase bone strength, in order to decrease the risk of fracture. In untreated men and women, BMD is one of the major determinants of bone strength, and low BMD is an important predictor of fracture. Whether the long-term anti-fracture efficacy of anti-osteoporotic drugs depends on the extent to which treatment can increase or maintain BMD is controversial [336]. Meta-regressions, based on summary statistics, demonstrate a stronger correlation between the change in BMD and fracture risk reduction than results based on the individual patient data [337, 338].
Whereas 16% of vertebral fracture risk reduction after treatment with alendronate was attributed to an increase in BMD at the lumbar spine [339], larger increases in BMD at both the spine and hip, observed with alendronate, were associated with greater reductions in the risk of non-vertebral fractures. However, for patients treated with risedronate or raloxifene, changes in BMD predict even more poorly the degree of reduction in vertebral (raloxifene) or non-vertebral (risedronate) fractures. Twelve percent and 7% of the effects of risedronate to reduce non-vertebral fractures were attributed to changes in the spine and femoral neck BMD, respectively [340]. For raloxifene, the percentage changes in BMD accounted for 4% of the observed vertebral fracture risk reduction [341]. Percent changes in total hip BMD at month 36 explained up to 35% of the effect of denosumab to reduce new or worsening vertebral fractures and up to 84% of the reduction in non-vertebral fracture risk [342]. It is reasonable to conclude, however, that early monitoring of BMD has limited value in the prediction of treatment responses with inhibitors of bone resorption.
For bone-forming agents, increases in BMD account for approximately one third of the vertebral fracture risk reduction with teriparatide [343]. Further data are needed on the role of BMD monitoring patients treated with bone-forming agents but appears to be of greater value than their use with inhibitors of bone resorption.
In postmenopausal osteoporosis, treatment-induced increments in BMD with inhibitors of bone turnover are modest (typically 2% per year) in comparison to the precision error of repeat measurements (typically 1–2%) so that the time interval of repeat estimates must be sufficiently long in order to determine whether any change is real [344]. In the absence of other clinical imperatives, a 5-year interval may be appropriate. For other agents such as and PTH derivatives, the treatment-induced increment is much more rapid and more frequent BMD tests may be considered.
Monitoring of treatment with biochemical markers of bone turnover
The most informative biochemical markers of bone turnover for the monitoring of osteoporosis are procollagen I N-terminal extension peptide (P1NP) for assessing bone formation, and C-telopeptide breakdown products (especially serum CTX) to assess bone resorption [72,73,74].
Treatment-induced changes in bone markers are more rapid than changes in BMD and are typically measured 3–6 months or so after starting treatment when treatment-induced changes are expected to be most evident. In a research setting, a significant association has been reported between the short-term decrease in markers of bone turnover with the use of anti-resoptive agents and gains in BMD [345, 346]. More importantly, significant associations have been reported between the short-term decrease in markers of bone turnover and the reduction in risk of vertebral and non-vertebral fractures with the use of anti-resorptive agents (raloxifene and bisphosphonates). For the bisphosphonates, a screening strategy has been proposed by the IOF based on the response of P1NP and CTX after 3 months of therapy [334]. If no change is observed, the clinician should reassess the adherence to the treatment and also other potential issues with the drug. More research is required using standardised analytes before robust evidence-based recommendations can be given [73].
Despite limited evidence, failure of treatment may be inferred when two or more incident fractures have occurred during treatment, when serial measurements of bone turnover markers are not suppressed by anti-resorptive therapy and where bone mineral density continues to decrease [347].
Investigation of patients with osteoporosis
Diagnostic work up
The same diagnostic approach should be undertaken in all patients with osteoporosis irrespective of the presence or absence of fragility fractures. However, the range of clinical and biological tests will depend on the severity of the disease, the age at presentation and the presence or absence of vertebral fractures. The aims of the clinical history, physical examination and clinical tests are as follows:
-
To exclude a disease which can mimic osteoporosis (e.g. osteomalacia, myelomatosis);
-
To elucidate causes of osteoporosis and contributory factors;
-
To assess the severity of osteoporosis to determine the prognosis of the disease, i.e. the risk of subsequent fractures;
-
To select the most appropriate form of treatment;
-
To perform baseline measurements for subsequent monitoring of treatment.
The procedures that may be relevant to the investigation of osteoporosis are shown in Table 10. These investigations may be used to:
-
Establish the diagnosis of osteoporosis (e.g. DXA or X-rays);
-
Establish the cause (e.g. thyroid function tests for hyperthyroidism, and urinary free cortisol for Cushing syndrome);
-
Establish differential diagnosis (e.g. protein electrophoresis for myeloma, and serum calcium and alkaline phosphatase for osteomalacia).
Investigations commonly conducted in secondary care include a full blood count, ESR, serum calcium and phosphate, liver function tests and tests of renal function. Additional measurements include the biochemical indices of bone turnover, serum parathyroid hormone, serum 25-hydroxyvitamin D, serum or urine protein electrophoresis, fasting and 24-h urinary calcium, urinary free cortisol, thyroid function tests, IgA anti-tissue transglutaminase antibody or IgA endomysial antibody, tryptase and (rarely) transiliac bone biopsy. Free testosterone, gonadotrophin and prolactin measurements may be of value in men. Assessment is guided by the clinical findings, and some patients who apparently have primary osteoporosis are subsequently found to have mild hyperparathyroidism or hyperthyroidism, systemic mastocytosis, the late appearance of osteogenesis imperfecta or osteomalacia.
Differential diagnosis of osteoporosis
Osteomalacia and malignancy commonly induce bone loss and fractures. Osteomalacia is characterised by a defect of mineralisation of bone matrix most commonly attributable to impaired intake, production or metabolism of vitamin D. Other causes include impaired phosphate transport or the chronic use of some drugs such as aluminium salts (and other phosphate binding antacids), high doses of fluoride or etidronate, and the chronic use of some anticonvulsants. In most cases, the diagnosis of osteomalacia is suspected by the clinical history and by abnormalities in biochemical tests such as low values of serum and urinary calcium, serum phosphate and 25-hydroxyvitamin D, and high values for alkaline phosphatase and parathyroid hormone. A transiliac bone biopsy after double tetracycline labelling may be necessary to demonstrate unequivocally a defect in mineralisation.
Diffuse osteoporosis with or without pathological fracture is common in patients with multiple myeloma, a condition suspected by the severity of bone pain, increased sedimentation rate and Bence Jones proteinuria and identified by marrow aspirate, and serum and urine (immuno-) electrophoresis of proteins. Similarly, pathological fractures resulting from metastatic malignancies can mimic osteoporosis and can be excluded by clinical and radiological examination, biological tests such as tumour markers, and scintigraphy or other imaging techniques. Vertebral fractures in osteoporosis should be differentiated from vertebral deformities attributable to other disorders such as scoliosis, osteoarthrosis and Scheuermann’s disease.
Health economics
There is an increasing need for management strategies to be placed in an appropriate health economic perspective for guideline development and for reimbursement. The type of evaluation used is principally cost-utility analysis as a measure of cost-effectiveness. In the context of evaluating treatments, this takes account, not only of fractures avoided, but also of any change in morbidity and mortality from both beneficial and unwanted effects. QALYs are the accepted unit of measurement in health economic assessment of interventions using cost-utility analysis. In order to estimate QALYs, each year of life is valued according to its utility to the patient. Values range from 0, the least desirable health state, to 1, or perfect health. The decrement in utility associated with fractures is the cumulative loss of utility over time. There is at present little international consensus as to when treatment can be considered to be cost-effective [348, 349]. One approach is to base the threshold value on a measure of a country’s economic performance and a value of about 2 times GDP/capita has been suggested as a threshold that can be applied to Western economies [350]. On this basis, threshold values would be about €32,000 in the UK, close to the recommendation of the National Institute for Health and Clinical Excellence [351]. Although the GDP per capita provides an index of affordability, there is also a marked heterogeneity in the proportion of GDP that countries are willing to devote to health care, and in the proportion of the population at risk from osteoporotic fracture (i.e. elderly people). In a systematic review, the ratio between WTP per QALY and GDP per capita varies widely from 0.05 to 5.40, depending on scenario outcomes. The average ratio of WTP per QALY and GDP per capita for extending life or saving life was 2.03 [352].
Studies of intervention
There has been a rapid expansion of research in Europe on the cost-utility of interventions in osteoporosis, which has been the subject of several reviews [124, 128, 353,354,355,356,357]. A useful tabular summary of studies up to April 2012 is provided in Brandão et al. [358]. Despite the use of different models, different settings and payer perspectives, analyses suggest that there are cost-effective scenarios that can be found in the context of the management of osteoporosis for all but the most expensive interventions (Table 11) [127]. A pan-European study from 2004 estimated the cost-effectiveness of branded alendronate in nine countries [359]. Alendronate was shown to be cost-saving compared to no treatment in women with osteoporosis (with and without previous vertebral fracture) from the Nordic countries (Norway, Sweden and Denmark). The cost-effectiveness of alendronate compared to no treatment was also within acceptable ranges in Belgium, France, Germany, Italy, Spain, Switzerland and the UK. However, with the markedly decrease in price of generic bisphosphonates, analyses based on a branded drug price have become obsolete. For example, the cost of alendronate (70 mg weekly) assumed in Table 11 was £95 per annum (2007) and in 2017 had fallen to a yearly cost of £8.64 in the UK. NICE have recently reappraised the cost-effectiveness of oral and intravenous bisphosphonates [128]. Treatment with oral bisphosphonates was cost-effective of women with a 10-year probability of a major osteoporotic fracture of 1% or more. For intravenous bisphosphonates, the threshold for cost-effectiveness was a 10-year probability of 10%.
The advent of probability-based assessment has prompted the cost-effectiveness of interventions as a function of fracture probability. Several studies have examined the cost-effectiveness of intervention thresholds expressed in terms of fracture probability [123, 127, 130, 360, 361]. In studies from the UK [114, 127], generic alendronate was shown to be cost-effective in the prevention and treatment of fractures in postmenopausal women with a 10-year fracture probability for a major fracture that exceeded 7.5% (Fig. 14). It is interesting that in the different European countries where such studies have been performed, the probabilities of major fractures selected as making generic alendronate a cost-effective intervention are quite similar: 7.5% in the UK [127], 8.8% in Portugal [363], 13.8% in Switzerland [361] and 10–15%, depending on age, in Greece [362]. This is quite remarkable, given the disparities in the clinical and economic epidemiology of factures and, especially, the willingness to pay adopted for each country: the UK €27,786, Switzerland €115,000, Portugal €32,000 and Greece €30,000.
Correlation between the 10-year probability of a major fracture (calculated with BMD) and cost-effectiveness of generic alendronate at the age of 50 years in women (BMI set to 26 kg/m2). Each point represents a particular combination of BMD and clinical risk factors (all possible combinations of CRFs at BMD T-scores between 0 and − 3.5 SD in 0.5 SD steps—512 combinations) with a BMI set to 26 kg/m2. The horizontal line denotes the threshold for cost-effectiveness (a willingness to pay of £20,000/QALY gained). From [114], with kind permission from Springer Science and Business Media
The recent appraisal by NICE [128] indicated that all oral bisphosphonates were cost-effective in women with a 10-year probability of 1% or more. Thus, the all treatment scenarios with alendronate can be considered as cost-effective (see Table 6 and Fig. 9). This raises an important issue in that the health economic thresholds espoused by NICE simply demarcate a level of risk above which the respective oral and IV bisphosphonate treatments are cost-effective but that the thresholds used to decide treatment should be based on clinical appropriateness [136, 364].
A special need for the incorporation of FRAX into health economic models arises from studies that have examined the interaction between FRAX-based probabilities with effectiveness. Interventions studied include raloxifene [195, 201], bazedoxifene [201], clodronate [365], daily and weekly teriparatide [366, 367], denosumab [368], alendronate [369], as well as a basket of interventions used by general practitioners in the UK [111]. Most of these were post hoc but, in the case of denosumab, was a pre-planned analysis. In addition, the ‘screening for prevention of fractures in older women’ (SCOOP) study was a prospective randomised study that demonstrated efficacy for hip fracture in women selected on the basis of hip fracture probability assessed using FRAX [111].
Several of these studies have shown greater efficacy against fracture in individuals at higher risk treated with clodronate, bazedoxifene, denosumab and in the SCOOP study. This FRAX-dependency has marked economic consequences, illustrated when comparing the cost-effectiveness of the two selective oestrogen receptor modulators, raloxifene and bazedoxifene. The overall effectiveness of these two agents on vertebral fracture risk is rather comparable but the efficacy of bazedoxifene increases in women with the higher the baseline fracture probability. In contrast, the relative risk reduction with raloxifene is constant over the range of fracture probabilities studied. As a consequence, raloxifene has better cost-effectiveness at low fracture probabilities whereas bazedoxifene has the better cost-effectiveness at high baseline fracture probabilities [370, 371]. The contrasting effect of FRAX-dependent and FRAX-independent interactions with efficacy on fractures averted is shown in Table 12.
Despite differences in apparent cost-effectiveness, there is, however, no proven difference in efficacy between the majority of treatments shown in Table 11 and head to head comparisons of interventions with fracture outcomes are few and recent [372]. For these reasons, the value of an incremental analysis between the individual treatments is questionable, since any resulting hierarchy of treatments is dependent largely on price, but otherwise meaningless in clinical terms. In addition, the large number of untreated patients makes ‘no treatment’ a relevant comparator. Notwithstanding, alendronate has been considered as a first line intervention. The view arises, not because of apparent differences in efficacy between treatments, but because of cost. However, the poor effectiveness and side effect profile of many generic formulations challenge this view [251].
The advent of new anabolic agents given for relatively short periods followed by maintenance with sequential inhibitors of bone resorption will offer new challenges for health economic appraisal.
Change history
31 October 2019
The original version of this article, published on 15 October 2018, unfortunately, contained a mistake.
18 February 2020
The article [European guidance for the diagnosis and management of osteoporosis in postmenopausal women], written by [J. A. Kanis], was originally published Online First without Open Access.
References
Kanis JA, Delmas P, Burckhardt P, Cooper C, Torgerson D (1997) Guidelines for diagnosis and management of osteoporosis. The European Foundation for Osteoporosis and Bone Disease. Osteoporos Int 7:390–406
Kanis JA, Burlet N, Cooper C, Delmas PD, Reginster JY, Borgstrom F, Rizzoli R (2008) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 19:399–428
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster J-Y, on behalf of the Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the Committee of Scientific Advisors of the International Osteoporosis Foundation (IOF) (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24:23–57
Hernlund E, Svedbom A, Ivergård M, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Archives of Osteoporosis 8:136. https://doi.org/10.1007/s11657-013-0136-1. Access: http://www.iofbonehealth.org/data-publications/regional-audits/osteoporosis-european-union-medical-management-epidemiology-and Accessed 4 Jan 2018
Kanis JA, Svedbom A, Harvey N, McCloskey EV (2014) The osteoporosis treatment gap. J Bone Miner Res 29:1926–1928
Kim SC, Kim DH, Mogun H, Eddings W, Polinski JM, Franklin JM, Solomon DH (2016) Impact of the U.S. Food and Drug Administration’s safety-related announcements on the use of bisphosphonates after hip fracture. J Bone Miner Res 31:1536–1540
Elliot-Gibson V, Bogoch ER, Jamal SA, Beaton DE (2004) Practice patterns in the diagnosis and treatment of osteoporosis after a fragility fracture: a systematic review. Osteoporos Int 15:767–778
Giangregorio L, Papaioannou A, Cranney A, Zytaruk N, Adachi JD (2006) Fragility fractures and the osteoporosis care gap: an international phenomenon. Semin Arthritis Rheum 35:293–305
Haaland DA, Cohen DR, Kennedy CC, Khalidi NA, Adachi JD, Papaioannou A (2009) Closing the osteoporosis care gap: increased osteoporosis awareness among geriatrics and rehabilitation teams. BMC Geriatr 9:28
Consensus Development Conference (1993) Diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med 94:646–650
World Health Organization (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser 843:1–129
Kanis JA on behalf of the WHO Scientific Group (2008) Assessment of osteoporosis at the primary health-care level. WHO Collaborating Centre, University of Sheffield, Sheffield, UK, Technical Report
Nguyen T, Sambrook P, Kelly P, Jones G, Lord S, Freund J, Eisman J (1993) Prediction of osteoporotic fractures by postural instability and bone density. BMJ 307:1111–1115
Kanis JA, Johnell O, Odén A, Sembo I, Redlund-Johnell I, Dawson A, De Laet C, Jonsson B (2000) Long-term risk of osteoporotic fracture in Malmo. Osteoporos Int 11:669–674
Cooper C, Atkinson EJ, Jacobsen SJ, O’Fallon WM, Melton LJ, 3rd (1993) Population-based study of survival after osteoporotic fractures. Am J Epidemiol 137:1001–1005
Kanis JA, Odén A, Johnell O, De Laet C, Jonsson B, Oglesby AK (2003) The components of excess mortality after hip fracture. Bone 32:468–473
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733
Blake G, Adams JE, Bishop N (2013) DXA in adults and children. Primer on the metabolic bone diseases and disorders of mineral metabolism, 8th edition. Ed Rosen CJ, Chapter 30, pp 249–263. John Wiley & Sons,
Glüer CC (2013) Quantitative computed tomography in children and adults. Primer on the metabolic bone diseases and disorders of mineral metabolism, 8th edition. Ed Rosen CJ, Chapter 31, pp 264–276. John Wiley & Sons,
Majumdar S (2013) Magnetic resonance imaging of bone. Primer on the metabolic bone diseases and disorders of mineral metabolism, 8th edition. Ed Rosen CJ, Chapter 32, pp 277–282. John Wiley & Sons,
Gary JR, Cook G, Gnanasegaran G, Fogelman I (2013) Radionuclide scintigraphy in metabolic bone disease. In: Primer on the metabolic bone diseases and disorders of mineral metabolism, 8th edition. Ed Rosen CJ, chapter 33, pp. John Wiley & Sons, pp 283–288
Johannesdottir F, Thrall E, Muller J, Keaveny TM, Kopperdahl DL, Bouxsein ML (2007) Comparison of non-invasive assessments of strength of the proximal femur. Bone 105:93–102
Silva BC, Leslie WD, Resch H, Lamy O, Lesnyak O, Binkley N, McCloskey EV, Kanis JA, Bilezikian JP (2014) Trabecular bone score: a non-invasive analytical method based upon the DXA image. J Bone Miner Res 29:518–530
Edmondson CP, Schwartz EN (2017) Non-BMD DXA measurements of the hip. Bone 104:73–83
Leslie WD, Lix LM, Majumdar SR, Morin SN, Johansson H, Odén A, McCloskey EV, Kanis JA (2017) Total hip bone area affects fracture prediction with FRAX in Canadian white women. J Clin Endocrinol Metab 102:4242–4249
Bala Y, Zebaze R, Ghasem-Zadeh A, Atkinson EJ, Iuliano S, Peterson JM, Amin S, Bjørnerem Å, Melton LJ 3rd, Johansson H, Kanis JA, Khosla S, Seeman E (2014) Cortical porosity identifies women with osteopenia at increased risk for forearm fractures. J Bone Miner Res 26:1356–1362
Zebaze R, Ghasem-Zadeh A, Mbala A, Seeman E (2013) A new method of segmentation of compact-appearing, transitional and trabecular compartments and quantification of cortical porosity from high resolution peripheral quantitative computed tomographic images. Bone 54:8–20
Schousboe JT, Ensrud KE, Nyman JA, Kane RL, Melton LJ, 3rd (2006) Cost-effectiveness of vertebral fracture assessment to detect prevalent vertebral deformity and select postmenopausal women with a femoral neck T-score >−2.5 for alendronate therapy: a modeling study. J Clin Densitom 9:133–143
McCloskey EV, Vasireddy S, Threlkeld J, Eastaugh J, Parry A, Bonnet N, Beneton M, Kanis JA, Charlesworth D (2008) Vertebral fracture assessment (VFA) with a densitometer predicts future fractures in elderly women unselected for osteoporosis. J Bone Miner Res 23:1561–1568
Lee JH, Lee YK, Oh SH, Ahn J, Lee YE, Pyo JH, Choi YY, Kim D, Bae SC, Sung YK, Kim DY (2016) A systematic review of diagnostic accuracy of vertebral fracture assessment (VFA) in postmenopausal women and elderly men. Osteoporos Int 27:1691–1699
Lewiecki EM (2010) Bone densitometry and vertebral fracture assessment. Curr Osteoporos Rep 8:123–130
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 312:1254–1259
Gluer CC (1997) Quantitative ultrasound techniques for the assessment of osteoporosis: expert agreement on current status. The International Quantitative Ultrasound Consensus Group. J Bone Miner Res 12:1280–1288
Kanis JA, Melton LJ 3rd, Christiansen C, Johnston CC, Khaltaev N (1994) The diagnosis of osteoporosis. J Bone Miner Res 9:1137–1141
Watts NB (2004) Fundamentals and pitfalls of bone densitometry using dual-energy X-ray absorptiometry (DXA). Osteoporos Int 15:847–854
Looker AC, Wahner HW, Dunn WL Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr., Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8: 468–489
Kanis JA, McCloskey EV, Johansson H, Odén A, Melton LJ, 3rd, Khaltaev N (2008) A reference standard for the description of osteoporosis. Bone 42: 467–475
Ferrari S, Bianchi ML, Eisman JA, Foldes AJ, Adami S, Wahl DA, Stepan JJ, de Vernejoul MC, Kaufman JM (2012) Osteoporosis in young adults: pathophysiology, diagnosis, and management. Osteoporos Int 23:2735–2748
Kanis JA, Gluer CC (2000) An update on the diagnosis and assessment of osteoporosis with densitometry. Committee of Scientific Advisors, International Osteoporosis Foundation. Osteoporos Int 11:192–202
De Laet CEDH, Van Hout BA, Burger H, Hofman A, Weel AE, Pols H (1998) Hip fracture prediction in elderly men and women: validation in the Rotterdam study. J Bone Miner Res 13: 1587–1593
Johnell O, Kanis JA, Odén A, Johansson H, De Laet C, Delmas P, Eisman JA, Fujiwara S, Kroger H, Mellstrom D, Meunier PJ, Melton LJ 3rd, O’Neill T, Pols H, Reeve J, Silman A, Tenenhouse A (2005) Predictive value of BMD for hip and other fractures. J Bone Miner Res 20: 1185–1194
Kanis JA, Bianchi G, Bilezikian JP, Kaufman JM, Khosla S, Orwoll E, Seeman E (2011) Towards a diagnostic and therapeutic consensus in male osteoporosis. Osteoporos Int 22:2789–2798
Lewiecki EM, Watts NB, McClung MR, Petak SM, Bachrach LK, Shepherd JA, Downs RW, Jr. (2004) Official positions of the international society for clinical densitometry. J Clin Endocrinol Metab 89:3651–3655
Binkley N, Bilezikian JP, Kendler DL, Leib ES, Lewiecki EM, Petak SM (2006) Official positions of the International Society for Clinical Densitometry and Executive Summary of the 2005 Position Development Conference. J Clin Densitom 9:4–14
Blake GM, Patel R, Knapp KM, Fogelman I (2003) Does the combination of two BMD measurements improve fracture discrimination? J Bone Miner Res 18:1955–1963
Kanis JA, Johnell O, Odén A, Johansson H, Eisman JA, Fujiwara S, Kroger H, Honkanen R, Melton LJ 3rd, O’Neill T, Reeve J, Silman A, Tenenhouse A (2006) The use of multiple sites for the diagnosis of osteoporosis. Osteoporos Int 17: 527–534
Leslie WD, Lix LM, Tsang JF, Caetano PA (2007) Single-site vs multisite bone density measurement for fracture prediction. Arch Intern Med 167:1641–1647
Odén A, McCloskey EV, Johansson H, Kanis JA (2013) Assessing the impact of osteoporosis on the burden of hip fractures. Calcif Tissue Int 92:42–49
Kanis JA, Johnell O, Odén A, Dawson A, De Laet C, Jonsson B (2001) Ten-year probabilities of osteoporotic fractures according to BMD and diagnostic thresholds. Osteoporos Int 12:989–995
Cummings SR, Black DM, Nevitt MC, Browner W, Cauley J, Ensrud K, Genant HK, Palermo L, Scott J, Vogt TM (1993) Bone density at various sites for prediction of hip fractures. The Study of Osteoporotic Fractures Research Group. Lancet 341:72–75
Moayyeri A, Adams JE, Adler RA, Krieg MA, Hans D, Compston J, Lewiecki EM (2012) Quantitative ultrasound of the heel and fracture risk assessment: an updated meta-analysis. Osteoporos Int 23:143–153
McCloskey EV, Kanis JA, Odén A, Harvey NC, Bauer D, González-Macias J, Hans D, Kaptoge S, Krieg MA, Kwok T, Marin F, Moayyeri A, Orwoll E, Gluёr C, Johansson H (2015) Predictive ability of heel quantitative ultrasound for incident fractures: an individual-level meta-analysis. Osteoporos Int 26:1979–1987
Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM (1995) Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med 332:767–773
Ribot C, Pouilles JM, Bonneu M, Tremollieres F (1992) Assessment of the risk of post-menopausal osteoporosis using clinical factors. Clin Endocrinol 36:225–228
Poor G, Atkinson EJ, O’Fallon WM, Melton LJ 3rd (1995) Predictors of hip fractures in elderly men. J Bone Miner Res 10:1900–1907
Kanis JA (2002) Diagnosis of osteoporosis and assessment of fracture risk. Lancet 359:1929–1936
Hui SL, Slemenda CW, Johnston C (1988) Age and bone mass as predictors of fracture in a prospective study. J Clin Invest 81:1804–1809
Kanis JA, Johansson H, Odén A, Johnell O, De Laet C, Eisman JA, McCloskey EV, Mellstrom D, Melton LJ 3rd, Pols HA, Reeve J, Silman AJ, Tenenhouse A (2004) A family history of fracture and fracture risk: a meta-analysis. Bone 35: 1029–1037
Kanis JA, Johansson H, Odén A, Johnell O, de Laet C, Melton LJ III, Tenenhouse A, Reeve J, Silman AJ, Pols HA, Eisman JA, McCloskey EV, Mellstrom D (2004) A meta-analysis of prior corticosteroid use and fracture risk. J Bone Miner Res 19:893–899
Kanis JA, Johansson H, Johnell O, Odén A, De Laet C, Eisman JA, Pols H, Tenenhouse A (2005) Alcohol intake as a risk factor for fracture. Osteoporos Int 16:737–742
Kanis JA, Johnell O, Odén A, Johansson H, De Laet C, Eisman J (2005) Smoking and fracture risk: a meta-analysis. Osteoporos Int 16:155–162
De Laet C, Kanis JA, Odén A, Johanson H, Johnell O, Delmas P, Eisman JA, Kroger H, Fujiwara S, Garnero P, McCloskey EV, Mellstrom D, Melton LJ 3rd, Meunier PJ, Pols HA, Reeve J, Silman A, Tenenhouse A (2005) Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int 16:1330–1338
Klotzbuecher CM, Ross PD, Landsman PD, Abbott TA, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15:721–739
Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P, Eisman J, Fujiwara S, Garnero P, Kroger H, McCloskey EV, Mellstrom D, Melton LJ, Pols H, Reeve J, Silman A, Tenenhouse A (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35:375–382
Kanis JA, McCloskey E, Johansson H, Odén A, Leslie WD (2012) FRAXwith and without bone mineral density. Calcif Tissue Int 90:1–13
Schwartz AV, Vittinghoff E, Bauer DC, Hillier TA, Strotmeyer ES, Ensrud KE, Donaldson MG, Cauley JA, Harris TB, Koster A, Womack CR, Palermo L, Black DM (2011) Association of BMD and FRAX score with risk of fracture in older adults with type 2 diabetes. JAMA 305:2184–2192
Giangregorio LM, Leslie WD, Lix LM, Johansson H, Odén A, McCloskey E, Kanis JA (2012) FRAX underestimates fracture risk in patients with diabetes. J Bone Miner Res 27:301–308
Leslie WD, Rubin MR, Schwartz AZ, Kanis JA (2012) Perspective: diabetes and bone. J Bone Miner Res 27:2231–2237
Nguyen ND, Frost SA, Center JR, Eisman JA, Nguyen TV (2008) Development of prognostic nomograms for individualizing 5-year and 10-year fracture risks. Osteoporos Int 19:1431–1444
Hippisley-Cox J, Coupland C (2009) Predicting risk of osteoporotic fracture in men and women in England and Wales: prospective derivation and validation of QFractureScores. BMJ 339:b4229
McClung MR, Geusens P, Miller PD, Zippel H, Bensen WG, Roux C, Adami S, Fogelman I, Diamond T, Eastell R, Meunier PJ, Reginster JY (2001) Effect of risedronate on the risk of hip fracture in elderly women. Hip Intervention Program Study Group. N Engl J Med 344:333–340
Delmas PD, Eastell R, Garnero P, Seibel MJ, Stepan J (2000) The use of biochemical markers of bone turnover in osteoporosis. Committee of Scientific Advisors of the International Osteoporosis Foundation. Osteoporos Int 11(Suppl 6):S2–17
Vasikaran S, Eastell R, Bruyère O, Foldes AJ, Garnero P, Griesmacher A, McClung M, Morris HA, Silverman S, Trenti T, Wahl DA, Cooper C, Kanis JA (2011) Markers of bone turnover for the prediction of fracture risk and monitoring of osteoporosis treatment: a need for international reference standards. Osteoporos Int 22:391–420
Johansson H, Odén A, Kanis JA, McCloskey EV, Morris HA, Cooper C, Vasikaran S (2014) A meta-analysis of reference markers of bone turnover for prediction of fracture. Calcif Tissue Int 94:560–567
Morris HA, Eastell R, Jorgensen NR, Cavalier E, Vasikaran S, Chubb SAP, Kanis JA, Cooper C, Makris K (2017) Clinical usefulness of bone turnover marker concentrations in osteoporosis. Clin Chim Acta 467:34–41
Harvey NC, Glüer CC, Binkley N, McCloskey EV, Brandi ML, Cooper C, Kendler D, Lamy O, Laslop A, Camargos BM, Reginster JY, Rizzoli R, Kanis JA (2015) Trabecular bone score (TBS) as a new complementary approach for osteoporosis evaluation in clinical practice. A consensus report of a European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) Working Group. Bone 78:216–224
McCloskey EV, Odén A, Harvey NC, Leslie WD, Hans D, Johansson H, Barkmann R, Boutroy S, Brown J, Chapurlat R, Elders PJ, Fujita Y, Glüer CC, Goltzman D, Iki M, Karlsson M, Kindmark A, Kotowicz M, Kurumatani N, Kwok T, Lamy O, Leung J, Lippuner K, Ljunggren Ö, Lorentzon M, Mellström D, Merlijn T, Oei L, Ohlsson C, Pasco JA, Rivadeneira F, Rosengren B, Sornay-Rendu E, Szulc P, Tamaki J, Kanis JA (2016) A meta-analysis of trabecular bone score in fracture risk prediction and its relationship to FRAX. J Bone Miner Res 31:940–948
Martineau P, Leslie WD, Johansson H, Odén A, McCloskey EV, Hans D, Kanis JA (2017) Clinical utility of using lumbar spine trabecular bone score to adjust fracture probability: the Manitoba BMD cohort. J Bone Miner Res 32:1568–1574
Leslie WD, Aubry-Rozier B, Lix LM, Morin SN, Majumdar SR, Hans D (2014) Spine bone texture assessed by trabecular bone score (TBS) predicts osteoporotic fractures in men: the Manitoba Bone Density Program. Bone 67:10–14
McCloskey EV, Odén A, Harvey NC, Leslie WD, Hans D, Johansson H, Kanis JA (2015) Adjusting fracture probability by trabecular bone score. Calcif Tissue Int 96:500–509
Leslie WD, Johansson H, Kanis JA, Lamy O, Odén A, McCloskey EV, Hans D (2014) Lumbar spine texture enhances 10-year fracture probability assessment. Osteoporos Int 25:2271–2277
Fink HA, Milavetz DL, Palermo L, Nevitt MC, Cauley JA, Genant HK (2005) What proportion of incident radiographic vertebral deformities is clinically diagnosed and vice versa? J Bone Miner Res 20:1216–1222
Melton LJ 3rd, Atkinson EJ, Cooper C, O’Fallon WM, Riggs BL (1999) Vertebral fractures predict subsequent fractures. Osteoporos Int 10:214–221
Johansson H, Odén A, McCloskey EV, Kanis JA (2014) Mild morphometric vertebral fractures predict vertebral fractures but not non-vertebral fractures. Osteoporos Int 25:235–241
Compston J, Cooper A, Cooper C, Gittoes N, Gregson C, Harvey N, Hope S, Kanis JA, McCloskey EV, Poole KES, Reid DM, Selby P, Thompson F, Thurston A, Vine N (2017) UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos 12:43
Kanis JA, Harvey NC, Johansson H, Odén A, McCloskey EV, Leslie WD (2017) Overview of fracture prediction tools. J Clin Densitom 20:360–367
Kanis JA, Johnell O, Odén A, Johansson H, McCloskey E (2008) FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19:385–397
Kanis JA, Johansson H, Odén A, Cooper C, EV l MC (2014) Worldwide uptake of FRAX. Arch Osteoporos 9:166. https://doi.org/10.1007/s11657-013-0166-8
Kanis JA, Harvey NC, Cooper C, Johansson H, Odén A, McCloskey EV (2016) A systematic review of intervention thresholds based on FRAX. Arch Osteoporos 11(1):25
Kanis JA, Odén A, Johnell O, Johansson H, De Laet C, Brown J, Burckhardt P, Cooper C, Christiansen C, Cummings S, Eisman JA, Fujiwara S, Glüer C, Goltzman D, Hans D, Krieg MA, La Croix A, McCloskey E, Mellstrom D, Melton LJ 3rd, Pols H, Reeve J, Sanders K, Schott AM, Silman A, Torgerson D, van Staa T, Watts NB, Yoshimura N (2007) The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int 18:1033–1046
Kanis JA, Johnell O, De Laet C, Jonsson B, Odén A, Ogelsby AK (2002) International variations in hip fracture probabilities: implications for risk assessment. J Bone Miner Res 17:1237–1244
Kanis JA, Hans D, Cooper C, Baim S, Bilezikian JP, Binkley N, Cauley JA, Compston JE, Dawson-Hughes B, El-Hajj Fuleihan G, Johansson H, Leslie WD, Lewiecki EM, Luckey M, Odén A, Papapoulos SE, Poiana C, Rizzoli R, Wahl DA, McCloskey EV (2011) Interpretation and use of FRAX in clinical practice. Osteoporos Int 22:2395–2411
Van Staa TP, Leufkens HG, Abenhaim L, Zhang B, Cooper C (2000) Use of oral corticosteroids and risk of fractures. J Bone Miner Res 15:993–1000
Harvey NC, Odén A, Orwoll E, Lapidus J, Kwok T, Karlsson MK, Rosengren BE, Ljunggren Ö, Cooper C, McCloskey E, Kanis JA, Ohlsson C, Mellström D, Johansson H (2018) Falls predict fractures independently of FRAX probability: a meta-analysis of the Osteoporotic Fractures in Men (MrOS) Study. J Bone Miner Res 33:510–516
Harvey NC, Johansson H, Odén A, Karlsson MK, Rosengren BE, Ljunggren Ö, Cooper C, McCloskey E, Kanis JA, Ohlsson C, Mellström D (2016) FRAX predicts incident falls in elderly men. Findings from MrOs Sweden. Osteoporos Int 27:267–274
Oliver D, Connelly JB, Victor CR, Shaw FE, Whitehead A, Genc Y, Vanoli A, Martin FC, Gosney MA (2007) Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and meta-analyses. BMJ 334:82
Kayan K, Johansson H, Odén A, Vasireddy S, Pande K, Orgee J, Kanis JA, McCloskey EV (2009) Can fall risk be incorporated into fracture risk assessment algorithms: a pilot study of responsiveness to clodronate. Osteoporos Int 20:2055–2061
Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, Lamb SE (2009) Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2:CD007146
Michael YL, Whitlock EP, Lin JS, Fu R, O’Connor EA, Gold R (2010) Primary care-relevant interventions to prevent falling in older adults: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med 153:815–825
Kanis JA, Johansson H, Odén A, McCloskey EV (2011) Guidance for the adjustment of FRAX according to the dose of glucocorticoids. Osteoporos Int 22:809–816
Leslie WD, Lix LM, Johansson H, Odén A, McCloskey E, Kanis JA (2011) Spine-hip discordance and fracture risk assessment: a physician-friendly FRAX enhancement. Osteoporos Int 22:839–847
Johansson H, Kanis JA, Odén A, Leslie WD, Fujiwara S, Glüer CC, Kroger H, LaCroix AZ, Lau E, Melton LJ 3rd, Eisman JA, O’Neill TW, Goltzman D, Reid DM, McCloskey E (2014) Impact of femoral neck and lumbar spine BMD discordances on FRAX probabilities in women: a meta-analysis of international cohorts. Calcif Tiss Int 95: 428–435
Leslie WD, Shevroja E, Johansson H, McCloskey EV, Harvey NC, Kanis JA, Hans D (2018) Risk-equivalent T-score adjustment using lumbar spine trabecular bone score (TBS): the Manitoba BMD Registry. Osteoporos Int 29:751–758
Leslie WD, Lix LM, Morin SN, Johansson H, Odén A, McCloskey EV, Kanis JA (2015) Adjusting hip fracture probability in men and women using hip axis length: the Manitoba Bone Density Database. J Clin Densitom 19:326–331
Masud T, Binkley N, Boonen S, Hannan MT. on behalf of the FRAX Position Conference members (2011) Can falls and frailty be used in FRAX? J Clin Densitom 14: 194–204
Johansson H, Odén A, Lorentzon M, McCloskey E, Kanis JA, Harvey NC, Karlsson MK, Mellstrom D (2015) Is the Swedish FRAX model appropriate for immigrants to Sweden? Osteoporos Int 26:2617–2622
Leslie WD, Johansson H, McCloskey EV, Harvey NC, Kanis JA, Hans D (2018) Comparison of methods for improving fracture risk assessment in diabetes: the Manitoba BMD Registry. J Bone Miner Res https://doi.org/10.1002/jbmr.3538 [Epub ahead of print]
Brennan SL, Leslie WD, Lix LM, Johansson H, Odén A, McCloskey E, Kanis JA (2014) FRAX provides robust fracture prediction regardless of socioeconomic status. Osteoporos Int 25:61–69
Leslie WD, Orwoll EW, Nielson CM, Morin SN, Majumdar SR, Johansson H, Odén A, McCloskey EV, Kanis JA (2014) Estimated lean mass and fat mass differentially affect femoral bone density and strength index but are not FRAX independent risk factors for fracture. J Bone Miner Res 29:2511–2519
Leslie WD, Lix LM, Johansson H, Odén A, McCloskey E, Kanis JA (2012) Does osteoporosis therapy invalidate FRAX for fracture prediction? J Bone Miner Res 27:1243–1251
Shepstone L, Lenaghan E, Cooper C, Clarke S, Fong-Soe-Khioe R, Fordham R, Gittoes N, Harvey I, Harvey N, Heawood A, Holland R, Howe A, Kanis J, Marshall T, O’Neill T, Peters T, Redmond N, Torgerson D, Turner D, McCloskey E (2018) A randomized controlled trial of screening in the community to reduce fractures in older women—the SCOOP Study. Lancet 391:741–747
McCloskey E, Johansson H, Harvey NC, Shepstone L, Lenaghan E, Fordham R, Harvey I, Howe A, Cooper C, Clarke S, Gittoes N, Heawood A, Holland R, Marshall T, O’Neill TW, Peters TJ, Redmond N, Torgerson D, Kanis JA (2018) Management of patients with high baseline hip fracture risk by FRAX reduces hip fractures—a post hoc analysis from the SCOOP Study. J Bone Miner Res 33:1020–1026
Ismail AA, Cooper C, Felsenberg D, Varlow J, Kanis JA, Silman AJ, O’Neill TW (1999) Number and type of vertebral deformities: epidemiological characteristics and relation to back pain and height loss. European Vertebral Osteoporosis Study Group. Osteoporos Int 9:206–213
Kanis JA, McCloskey EV, Johansson H, Strom O, Borgstrom F, Odén A (2008) Case finding for the management of osteoporosis with FRAX—assessment and intervention thresholds for the UK. Osteoporos Int 19:1395–1408
Papaioannou A, Morin S, Cheung AM, Atkinson S, Brown JP, Feldman S, Hanley DA, Hodsman A, Jamal SA, Kaiser SM, Kvern B, Siminoski K, Leslie WD; Scientific Advisory Council of Osteoporosis Canada (2010) 2010 Clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ 182: 1864–1873
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, Lindsay R (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25:2359–2381
Kanis JA, Johnell O (2005) Requirements for DXA for the management of osteoporosis in Europe. Osteoporos Int 16:229–238
Kanis JA, McCloskey EV, Harvey NC, Johansson H, Leslie WD (2015) Intervention thresholds and the diagnosis of osteoporosis. J Bone Miner Res 30:1747–1753
Grigorie D, Sucaliuc A, Johansson H, Kanis JA, McCloskey E (2013) Incidence of hip fracture in Romania and the development of a Romanian FRAX model. Calcif Tissue Int 92:429–436
Johansson H, Azizieh F, Al Ali N, Alessa T, Harvey NC, McCloskey E, Kanis JA (2017) FRAX- vs. T-score-based intervention thresholds for osteoporosis. Osteoporos Int 28:3099–3105
Compston J, Cooper A, Cooper C, Francis R, Kanis JA, Marsh D, McCloskey EV, Reid DM, Selby P, Wilkins M (2009) Guidelines for the diagnosis and management of osteoporosis in postmenopausal women and men from the age of 50 years in the UK. Maturitas 62:105–108
Tarantino U, Iolascon G, Cianferotti L, Masi L, Marcucci G, Giusti F, Marini F, Parri S, Feola M, Rao C, Piccirilli E, Zanetti EB, Cittadini N, Alvaro R, Moretti A, Calafiore D, Toro G, Gimigliano F, Resmini G, Brandi ML (2017) Clinical guidelines for the prevention and treatment of osteoporosis: summary statements and recommendations from the Italian Society for Orthopaedics and Traumatology. J Orthop Traumatol 18(Suppl 1):3–36
Lekamwasam S, Adachi JD, Agnusdei D, Bilezikian J, Boonen S, Borgström F, Cooper C, Diez Perez A, Eastell R, Hofbauer LC, Kanis JA, Langdahl BL, Lesnyak O, Lorenc R, McCloskey E, Messina OD, Napoli N, Obermayer-Pietsch B, Ralston SH, Sambrook PN, Silverman S, Sosa M, Stepan J, Suppan G, Wahl DA, Compston JE (2012) A framework for the development of guidelines for the management of glucocorticoid-induced osteoporosis. Osteoporos Int 23:2257–2276
Kanis JA, Stevenson M, McCloskey EV, Davis S, Lloyd-Jones M (2007) Glucocorticoid-induced osteoporosis: a systematic review and cost-utility analysis. Health Technol Assess 11:1–256
Johansson H, Odén A, Johnell O, Jonsson B, de Laet C, Oglesby A, McCloskey EV, Kayan K, Jalava T, Kanis JA (2004) Optimization of BMD measurements to identify high risk groups for treatment—a test analysis. J Bone Miner Res 19:906–913
Johansson H, Kanis JA, Odén A, Johnell O, McCloskey E (2009) BMD, clinical risk factors and their combination for hip fracture prevention. Osteoporos Int 20:1675–1682
Kanis JA, Adams J, Borgstrom F, Cooper C, Jönsson B, Preedy D, Selby P, Compston J (2008) The cost-effectiveness of alendronate in the management of osteoporosis. Bone 42:4–15
National Institute for Health and Care Excellence (2017) TA 464: bisphosphonates for treating osteoporosis. Technology appraisal guidance 464. National Institute for Health and Care Excellence, London. nice.org.uk/guidance/ta464
Shiroiwa T, Sung YK, Fukuda T, Lang HC, Bae SC, Tsutani K (2010) International survey on willingness-to-pay (WTP) for one additional QALY gained: what is the threshold of cost effectiveness? Health Econ 19:422–437
Tosteson AN, Melton LJ, 3rd, Dawson-Hughes B, Baim S, Favus MJ, Khosla S, Lindsay RL (2008) Cost-effective osteoporosis treatment thresholds: the United States perspective. Osteoporos Int 19:437–447
Leslie WD, Morin S, Lix LM, Johansson H, Odén A, McCloskey E, Kanis JA (2012) Fracture risk assessment without bone density measurement in routine clinical practice. Osteoporos Int 23:75–85
Leslie WD, Majumdar SR, Lix LM, Johansson H, Odén A, McCloskey E, Kanis JA (2012) High fracture probability with FRAX usually indicates densitometric osteoporosis: implications for clinical practice. Osteoporos Int 23:391–397
McCloskey EV, Johansson H, Harvey NC, Compston J, Kanis JA (2017) Access to fracture risk assessment by FRAX® and linked National Osteoporosis Guideline Group (NOGG) guidance in the UK—an analysis of anonymous website activity. Osteoporos Int 28:71–76
McCloskey E, Kanis JA, Johansson H, Harvey N, Odén A, Cooper A, Cooper C, Francis RM, Reid DM, Marsh D, Selby P, Thompson F, Hewitt S, Compston J (2015) FRAX-based assessment and intervention thresholds—an exploration of thresholds in women aged 50 years and older in the UK. Osteoporos Int 26:2091–2099
Neuerburg C, Stumpf U, Schmidmaier R, Kammerlander C, Pfeilschifter J, Mutschler W, Bocker W (2017) Investigation and management of osteoporosis in aged trauma patients: a treatment algorithm adapted to the German guidelines for osteoporosis. J Orthop Surg Res 12:86. https://doi.org/10.1186/s13018-017-0585-0
Harvey NC, McCloskey E, Kanis JA, Compston J, Cooper C (2018) Cost-effective but clinically inappropriate: new NICE intervention thresholds in osteoporosis (Technology Appraisal 464). Osteoporos Int 29:1511–1513
Kanis JA, Odén A, Johansson H, McCloskey E (2012) Pitfalls in the external validation of FRAX. Osteoporos Int 23:423–431
Turner DA, Khioe RFS, Shepstone L, Lenaghan E, Cooper C, Gittoes N, Harvey NC, Holland R, Howe A, McCloskey E, O’Neill TW, Torgerson D, Fordham R (2018) The cost-effectiveness of screening in the community to reduce osteoporotic fractures in older women in the UK: economic evaluation of the SCOOP study. J Bone Miner Res 33:845–851
Howe TE, Shea B, Dawson LJ, Downie F, Murray A, Ross C, Harbour RT, Caldwell LM, Creed G (2011) Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev CD000333
Sañudo B, de Hoyo M, Del Pozo-Cruz J, Carrasco L, Del Pozo-Cruz B, Tejero S, Firth E (2017) Systematic review of the exercise effect on bone health: the importance of assessing mechanical loading in perimenopausal and postmenopausal women. Menopause 24: 1208–1216,
McMillan LB, Zengin A, Ebeling PR, Scott D (2017) Prescribing physical activity for the prevention and treatment of osteoporosis in older adults. Healthcare (Basel) 6;5(4). pii: E85. https://doi.org/10.3390/healthcare5040085
Howe TE, Rochester L, Neil F, Skelton DA, Ballinger C (2011) Exercise for improving balance in older people. Cochrane Database Syst Rev 11:CD004963
Sherrington C, Michaleff ZA, Fairhall N, Paul SS, Tiedemann A, Whitney J, Cumming RG, Herbert RD, Close JCT, Lord SR (2017) Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med 51:1750–1758
Tricco AC, Thomas SM, Veroniki AA, Hamid JS, Cogo E, Strifler L, Khan PA, Robson R, Sibley KM, MacDonald H, Riva JJ, Thavorn K, Wilson C, Holroyd-Leduc J, Kerr GD, Feldman F, Majumdar SR, Jaglal SB, Hui W, Straus SE (2017) Comparisons of interventions for preventing falls in older adults: a systematic review and meta-analysis. JAMA 318:1687–1699
El-Khoury F, Cassou B, Charles MA, Dargent-Molina P (2013) The effect of fall prevention exercise programmes on fall induced injuries in community dwelling older adults: systematic review and meta-analysis of randomised controlled trials. BMJ 347:f6234
Jepsen DB, Thomsen K, Hansen S, Jørgensen NR, Masud T, Ryg J (2017) Effect of whole-body vibration exercise in preventing falls and fractures: a systematic review and meta-analysis. BMJ Open 7(12):e018342
Sawka AM, Boulos P, Beattie K, Thabane L, Papaioannou A, Gafni A, Cranney A, Zytaruk N, Hanley DA, Adachi JD (2005) Do hip protectors decrease the risk of hip fracture in institutional and community-dwelling elderly? A systematic review and meta-analysis of randomized controlled trials. Osteoporos Int 16:1461–1474
Parker MJ, Gillespie WJ, Gillespie LD (2006) Effectiveness of hip protectors for preventing hip fractures in elderly people: systematic review. BMJ 332:571–574
Kiel DP, Magaziner J, Zimmerman S, Ball L, Barton BA, Brown KM, Stone JP, Dewkett D, Birge SJ (2007) Efficacy of a HIP protector to prevent HIP fracture in nursing home residents: the HIP PRO randomized controlled trial. JAMA 298:413–422
Gillespie WJ, Gillespie LD, Parker MJ (2010) Hip protectors for preventing hip fractures in older people. Cochrane Database Syst Rev CD001255
Rizzoli R (2014) Nutritional aspect of bone health. Best Pract Res Clin Endocrinol Metab 28:795–808
Food and Agricultural Organization of the United Nations/World Health Organization (2001) Human vitamin and mineral requirements. Report of a joint FAO/WHO expert consultation. Bangkok, Thailand. Washington, DC
Harvey NC, Biver E, Kaufman JM, Bauer J, Branco J, Brandi ML, Bruyère O, Coxam V, Cruz-Jentoft A, Czerwinski E, Dimai H, Fardellone P, Landi F, Reginster JY, Dawson-Hughes B, Kanis JA, Rizzoli R, Cooper C (2017) The role of calcium supplementation in healthy musculoskeletal ageing: an expert consensus meeting of the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) and the International Foundation for Osteoporosis (IOF). Osteoporos Int 28:447–462
Tang BM, Eslick GD, Nowson C, Smith C, Bensoussan A (2007) Use of calcium or calcium in combination with vitamin D supplementation to prevent fractures and bone loss in people aged 50 years and older: a meta-analysis. Lancet 370:657–666
Weaver CM, Alexander DD, Boushey CJ, Dawson-Hughes B, Lappe JM, LeBoff MS, Liu S, Looker AC, Wallace TC, Wang DD (2016) Calcium plus vitamin D supplementation and risk of fractures: an updated meta-analysis from the National Osteoporosis Foundation. Osteoporos Int 27:367–376
Zhao JG, Zeng XT, Wang J, Liu L (2017) Association between calcium or vitamin D supplementation and fracture incidence in community-dwelling older adults: a systematic review and meta-analysis. JAMA 318:2466–2482
Bolland MJ, Grey A, Avenell A, Gamble GD, Reid IR (2011) Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women’s Health Initiative limited access dataset and meta-analysis. BMJ 342:d2040
Nordin BE, Lewis JR, Daly RM, Horowitz J, Metcalfe A, Lange K, Prince RL (2011) The calcium scare—what would Austin Bradford Hill have thought? Osteoporos Int 22:3073–3077
Bolland MJ, Grey A, Reid IR (2011) Re: The calcium scare: what would Austin Bradford Hill have thought? Osteoporos Int 22:3079–3080 author reply 3081-3073
Bolland MJ, Grey A, Reid IR (2012) Misclassification does not explain increased cardiovascular risks of calcium supplements. J Bone Miner Res 27:959 author reply 960-951
Lewis JR, Calver J, Zhu K, Flicker L, Prince RL (2011) Calcium supplementation and the risks of atherosclerotic vascular disease in older women: results of a 5-year RCT and a 4.5-year follow-up. J Bone Miner Res 26:35–41
Lewis JR, Zhu K, Prince RL (2012) Adverse events from calcium supplementation: relationship to errors in myocardial infarction self-reporting in randomized controlled trials of calcium supplementation. J Bone Miner Res 27:719–722
Lewis JR, Zhu K, Prince RL (2012) Response to: Misclassification does not explain increased cardiovascular risks of calcium supplements. J Bone Miner Res 27:960–961
Hiligsmann M, Ben Sedrine W, Bruyère O, Evers SM, Rabenda V, Reginster JY (2015) Cost-effectiveness of vitamin D and calcium supplementation in the treatment of elderly women and men with osteoporosis. Europ J Public Health 25:20–25
Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB, Orav JE, Stuck AE, Theiler R, Wong JB, Egli A, Kiel DP, Henschkowski J (2009) Fall prevention with supplemental and active forms of vitamin D: a meta-analysis of randomised controlled trials. BMJ 339:b3692
Bischoff-Ferrari HA, Willett WC, Orav EJ, Lips P, Meunier PJ, Lyons RA, Flicker L, Wark J, Jackson RD, Cauley JA, Meyer HE, Pfeifer M, Sanders KM, Stähelin HB, Theiler R, Dawson-Hughes B (2012) Pooled analysis of vitamin D dose requirements for fracture prevention. N Engl J Med 367:40–49
Smith H, Anderson F, Raphael H, Maslin P, Crozier S, Cooper C (2007) Effect of annual intramuscular vitamin D on fracture risk in elderly men and women—a population-based, randomized, double-blind, placebo-controlled trial. Rheumatol (Oxford) 46:1852–1857
Sanders KM, Stuart AL, Williamson EJ, Simpson JA, Kotowicz MA, Young D, Nicholson GC (2010) Annual high-dose oral vitamin D and falls and fractures in older women: a randomized controlled trial. JAMA 303:1815–1822
Bischoff-Ferrari HA, Dawson-Hughes B, Orav EJ, Staehelin HB, Meyer OW, Theiler R, Dick W, Willett WC, Egli A (2016) Monthly high-dose vitamin D treatment for the prevention of functional decline: a randomized clinical trial. JAMA Intern Med 176:175–183
Smith LM, Gallagher JC, Suiter C (2017) Medium doses of daily vitamin D decrease falls and higher doses of daily vitamin D3 increase falls: a randomized clinical trial. J Steroid Biochem Mol Biol 173:317–322
Rizzoli R, Biver E, Bonjour J-P, Coxam V, Goltzman D, Kanis JA, Lappe J, Rejnmark L, Sahni S, Weaver C, Weiler H, Reginster JY (2018) Benefits and safety of dietary protein for bone health. A position paper from the International Osteoporosis Foundation and from the European Society for Clinical and Economical Aspects of Osteopororosis, Osteoarthritis and Musculoskeltal Diseases. Osteoporos Int May 8. https://doi.org/10.1007/s00198-018-4534-5. [Epub ahead of print]
Rizzoli R (2014) Dairy products, yogurts, and bone health. Am J Clin Nutr 99(5 Suppl):1256S–1262S
Rozenberg S, Body JJ, Bruyère O, Bergmann P, Brandi ML, Cooper C, Devogelaer JP, Gielen E, Goemaere S, Kaufman JM, Rizzoli R, Reginster JY (2016) Effects of dairy products consumption on health: benefits and beliefs—a commentary from the Belgian Bone Club and the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases. Calcif Tissue Int 98:1–17
Durosier-Izart C, Biver E, Merminod F, van Rietbergen B, Chevalley T, Herrmann FR, Ferrari SL, Rizzoli R (2017) Peripheral skeleton bone strength is positively correlated with total and dairy protein intakes in healthy postmenopausal women. Am J Clin Nutr 105:513–525
Langsetmo L, Shikany JM, Burghardt AJ, Cawthon PM, Orwoll ES, Cauley JA, Taylor BC, Schousboe JT, Bauer DC, Vo TN, Ensrud KE, Osteoporotic Fractures in Men (MrOS) Study Research Group (2018) High dairy protein intake is associated with greater bone strength parameters at the distal radius and tibia in older men: a cross-sectional study. Osteoporos Int 29:69–77
Feskanich D, Meyer HE, Fung TT, Bischoff-Ferrari HA, Willett WC (2018) Milk and other dairy foods and risk of hip fracture in men and women. Osteoporos Int 29:385–396
Laird E, Molloy AM, McNulty H, Ward M, McCarroll K, Hoey L, Hughes CF, Cunningham C, Strain JJ, Casey MC (2017) Greater yogurt consumption is associated with increased bone mineral density and physical function in older adults. Osteoporos Int 28:2409–2419
Rizzoli R, Biver E (2018) Effects of fermented milk products on bone. Calcif Tissue Int 102:489–500
Biver E, Durosier-Izart C, Merminod F, Chevalley T, van Rietbergen B, Ferrari SL, Rizzoli R (2018) Fermented dairy products consumption is associated with attenuated cortical bone loss independently of total calcium, protein, and energy intakes in healthy postmenopausal women. Osteoporos Int 29:1771–1782
Chen GC, Wang Y, Tong X, Szeto IMY, Smit G, Li ZN, Qin LQ (2017) Cheese consumption and risk of cardiovascular disease: a meta-analysis of prospective studies. Eur J Nutr 56:2565–2575
Ethgen O, Hiligsmann M, Burlet N, Reginster JY (2015) Public health impact and cost-effectiveness of dairy products supplemented with vitamin D in prevention of osteoporotic fractures. Arch Public Health 2015(14):73–48
Ethgen O, Hiligsmann M, Burlet N, Reginster JY (2016) Cost-effectiveness of personalized supplementation with vitamin D-rich dairy products. Osteoporos Int 27:301–308
Hiligsmann M, Neuprez A, Buckinx F, Locquet M, Reginster JY (2017) A scoping review of the public health impact of vitamin D-fortified dairy products for fracture prevention. Arch Osteoporos 12:57. https://doi.org/10.1007/s11657-017-0352-1
Hiligsmann M, Reginster JY (2017) The projected public health and economic impact of vitamin D fortified dairy products for fracture prevention in France. Expert Rev Pharmacoecon Outcomes Res 7:1–5
Saito T, Sterbenz JM, Malay S, Zhong L, MacEachern MP, Chung KC (2017) Effectiveness of anti-osteoporotic drugs to prevent secondary fragility fractures: systematic review and meta-analysis. Osteoporos Int 28:3289–3300
Kanis JA, Cooper C, Rizzoli R, Abrahamsen B, Al-Daghri NM, Brandi ML, Cannata-Andia J, Cortet B, Dimai HP, Ferrari S, Hadji P, Harvey NC, Kraenzlin M, Kurth A, McCloskey E, Minisola S, Thomas T, Reginster JY (2017) Identification and management of patients at increased risk of osteoporotic fracture: outcomes of an ESCEO expert consensus meeting. Osteoporos Int 28:2023–2034
Love RR, Mazess RB, Barden HS, Epstein S, Newcomb PA, Jordan VC, Carbone PP, DeMets DL (1992) Effects of tamoxifen on bone mineral density in postmenopausal women with breast cancer. N Engl J Med 326:852–856
Ettinger B, Black DM, Mitlak BH, Knickerbocker RK, Nickelsen T, Genant HK, Christiansen C, Delmas PD, Zanchetta JR, Stakkestad J, Glüer CC, Krueger K, Cohen FJ, Eckert S, Ensrud KE, Avioli LV, Lips P, Cummings SR (1999) Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) Investigators. JAMA 282:637–645
Delmas PD, Genant HK, Crans GG, Stock JL, Wong M, Siris E, Adachi JD (2003) Severity of prevalent vertebral fractures and the risk of subsequent vertebral and nonvertebral fractures: results from the MORE trial. Bone 33:522–532
Cummings SR, Eckert S, Krueger KA, Grady D, Powles TJ, Cauley JA, Norton L, Nickelsen T, Bjarnason NH, Morrow M, Lippman ME, Black D, Glusman JE, Costa A, Jordan VC (1999) The effect of raloxifene on risk of breast cancer in postmenopausal women: results from the MORE randomized trial. Multiple Outcomes of Raloxifene Evaluation. JAMA 281:2189–2197
Vogel VG, Costantino JP, Wickerham DL, Cronin WM, Cecchini RS, Atkins JN, Bevers TB, Fehrenbacher L, Pajon ER Jr, Wade JL 3rd, Robidoux A, Margolese RG, James J, Lippman SM, Runowicz CD, Ganz PA, Reis SE, McCaskill-Stevens W, Ford LG, Jordan VC, Wolmark N (2006) Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA 295:2727–2741
Mosca L, Barrett-Connor E, Wenger NK, Collins P, Grady D, Kornitzer M, Moscarelli E, Paul S, Wright TJ, Helterbrand JD, Anderson PW (2001) Design and methods of the Raloxifene Use for The Heart (RUTH) study. Am J Cardiol 88:392–395
Barrett-Connor E, Mosca L, Collins P, Geiger MJ, Grady D, Kornitzer M, McNabb MA, Wenger NK (2006) Effects of raloxifene on cardiovascular events and breast cancer in postmenopausal women. N Engl J Med 355:125–137
Kanis JA, Johnell O, Black DM, Downs RW Jr, Sarkar S, Fuerst T, Secrest RJ, Pavo I (2003) Effect of raloxifene on the risk of new vertebral fracture in postmenopausal women with osteopenia or osteoporosis: a reanalysis of the Multiple Outcomes of Raloxifene Evaluation trial. Bone 33:293–300
Kanis JA, Johansson H, Odén A, McCloskey EV (2010) A meta-analysis of the efficacy of raloxifene on all clinical and vertebral fractures and its dependency on FRAX. Bone 47:729–735
Silverman SL, Christiansen C, Genant HK, Vukicevic S, Zanchetta JR, de Villiers TJ, Constantine GD, Chines AA (2008) Efficacy of bazedoxifene in reducing new vertebral fracture risk in postmenopausal women with osteoporosis: results from a 3-year, randomized, placebo-, and active-controlled clinical trial. J Bone Miner Res 23:1923–1934
Silverman SL, Chines AA, Kendler DL, Kung AW, Teglbjaerg CS, Felsenberg D, Mairon N, Constantine GD, Adachi JD (2012) Sustained efficacy and safety of bazedoxifene in preventing fractures in postmenopausal women with osteoporosis: results of a 5-year, randomized, placebo-controlled study. Osteoporos Int 23:351–363
Palacios S, Silverman SL, de Villiers TJ, Levine AB, Goemaere S, Brown JP, De Cicco Nardone F, Williams R, Hines TL, Mirkin S, Chines AA, Bazedoxifene Study Group (2015) A 7-year randomized, placebo-controlled trial assessing the long-term efficacy and safety of bazedoxifene in postmenopausal women with osteoporosis: effects on bone density and fracture. Menopause 22:806–813
Ellis AG, Reginster JY, Luo X, Bushmakin AG, Williams R, Sutradhar S, Mirkin S, Jansen JP (2014) Indirect comparison of bazedoxifene vs oral bisphosphonates for the prevention of vertebral fractures in postmenopausal osteoporotic women. Curr Med Res Opin 30:1617–1626
Ellis AG, Reginster JY, Luo X, Cappelleri JC, Chines A, Sutradhar S, Jansen JP (2014) Bazedoxifene versus oral bisphosphonates for the prevention of nonvertebral fractures in postmenopausal women with osteoporosis at higher risk of fracture: a network meta-analysis. Value Health 17:424–432
Kanis JA, Johansson H, Odén A, McCloskey EV (2009) Bazedoxifene reduces vertebral and clinical fractures in postmenopausal women at high risk assessed with FRAX. Bone 44:1049–1054
de Villiers TJ, Chines AA, Palacios S, Lips P, Sawicki AZ, Levine AB, Codreanu C, Kelepouris N, Brown JP (2011) Safety and tolerability of bazedoxifene in postmenopausal women with osteoporosis: results of a 5-year, randomized, placebo-controlled phase 3 trial. Osteoporos Int 22:567–576
Umland EM, Karel L, Santoro N (2016) Bazedoxifene and conjugated equine estrogen: a combination product for the management of vasomotor symptoms and osteoporosis prevention associated with menopause. Pharmacotherapy 36:548–561
Hadji P, Ryan KA, Yu CR, Mirkin S, Komm BS (2016) CE/BZA effects on bone and quality of life in European postmenopausal women: a pooled analysis. Climacteric 19:482–487
Rizzoli R (2011) Bisphosphonates for post-menopausal osteoporosis: are they all the same? Quart J Med 104:281–300
Khan SA, Kanis JA, Vasikaran S, Kline WF, Matuszewski BK, McCloskey EV, Beneton MN, Gertz BJ, Sciberras DG, Holland SD, Orgee J, Coombes GM, Rogers SR, Porras AG (1997) Elimination and biochemical responses to intravenous alendronate in postmenopausal osteoporosis. J Bone Miner Res 12:1700–1707
Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, Bauer DC, Genant HK, Haskell WL, Marcus R, Ott SM, Torner JC, Quandt SA, Reiss TF, Ensrud KE (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet 348:1535–1541
Cranney A, Guyatt G, Griffith L, Wells G, Tugwell P, Rosen C (2002) Meta-analyses of therapies for postmenopausal osteoporosis. IX: summary of meta-analyses of therapies for postmenopausal osteoporosis. Endocr Rev 23:570–578
Stevenson M, Jones ML, De Nigris E, Brewer N, Davis S, Oakley J (2005) A systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosis. Health Technol Assess 9:1–160
Cummings SR, Black DM, Thompson DE, Applegate WB, Barrett-Connor E, Musliner TA, Palermo L, Prineas R, Rubin SM, Scott JC, Vogt T, Wallace R, Yates AJ, LaCroix AZ (1998) Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the Fracture Intervention Trial. JAMA 280:2077–2082
Axelsson KF, Wallander M, Johansson H, Lundh D, Lorentzon M (2017) Hip fracture risk and safety with alendronate treatment in the oldest-old. J Intern Med 282:546–559
Harris ST, Watts NB, Genant HK, McKeever CD, Hangartner T, Keller M, Chesnut CH 3rd, Brown J, Eriksen EF, Hoseyni MS, Axelrod DW, Miller PD (1999) Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. Vertebral Efficacy with Risedronate Therapy (VERT) Study Group. JAMA 282:1344–1352
Reginster J, Minne HW, Sorensen OH, Hooper M, Roux C, Brandi ML, Lund B, Ethgen D, Pack S, Roumagnac I, Eastell R (2000) Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Vertebral Efficacy with Risedronate Therapy (VERT) Study Group. Osteoporos Int 11:83–91
McClung MR, Balske A, Burgio DE, Wenderoth D, Recker RR (2013) Treatment of postmenopausal osteoporosis with delayed-release risedronate 35 mg weekly for 2 years. Osteoporos Int 24:301–310
Chesnut IC, Skag A, Christiansen C, Recker R, Stakkestad JA, Hoiseth A, Felsenberg D, Huss H, Gilbride J, Schimmer RC, Delmas PD (2004) Effects of oral ibandronate administered daily or intermittently on fracture risk in postmenopausal osteoporosis. J Bone Miner Res 19:1241–1249
Delmas PD, Recker RR, Chesnut CH, 3rd, Skag A, Stakkestad JA, Emkey R, Gilbride J, Schimmer RC, Christiansen C (2004) Daily and intermittent oral ibandronate normalize bone turnover and provide significant reduction in vertebral fracture risk: results from the BONE study. Osteoporos Int 15: 792–798
Harris ST, Blumentals WA, Miller PD (2008) Ibandronate and the risk of non-vertebral and clinical fractures in women with postmenopausal osteoporosis: results of a meta-analysis of phase III studies. Curr Med Res Opin 24:237–245
Reginster JY, Adami S, Lakatos P, Greenwald M, Stepan JJ, Silverman SL, Christiansen C, Rowell L, Mairon N, Bonvoisin B, Drezner MK, Emkey R, Felsenberg D, Cooper C, Delmas PD, Miller PD (2006) Efficacy and tolerability of once-monthly oral ibandronate in postmenopausal osteoporosis: 2 year results from the MOBILE study. Ann Rheum Dis 65:654–661
Miller PD, Recker RR, Reginster JY, Riis BJ, Czerwinski E, Masanauskaite D, Kenwright A, Lorenc R, Stakkestad JA, Lakatos P (2012) Efficacy of monthly oral ibandronate is sustained over 5 years: the MOBILE long-term extension study. Osteoporos Int 23:1747–1756
Delmas PD, Adami S, Strugala C, Stakkestad JA, Reginster JY, Felsenberg D, Christiansen C, Civitelli R, Drezner MK, Recker RR, Bolognese M, Hughes C, Masanauskaite D, Ward P, Sambrook P, Reid DM (2006) Intravenous ibandronate injections in postmenopausal women with osteoporosis: one-year results from the dosing intravenous administration study. Arthritis Rheum 54:1838–1846
Bianchi G, Czerwinski E, Kenwright A, Burdeska A, Recker RR, Felsenberg D (2012) Long-term administration of quarterly IV ibandronate is effective and well tolerated in postmenopausal osteoporosis: 5-year data from the DIVA study long-term extension. Osteoporos Int 23:1769–1778
Miller PD, Recker RR, Harris S, Silverman S, Felsenberg D, Reginster J, Day BM, Barr C, Masanauskaite D (2014) Long-term fracture rates seen with continued ibandronate treatment: pooled analysis of DIVA and MOBILE long-term extension studies. Osteoporos Int 25:349–357
Reid IR, Brown JP, Burckhardt P, Horowitz Z, Richardson P, Trechsel U, Widmer A, Devogelaer JP, Kaufman JM, Jaeger P, Body JJ, Brandi ML, Broell J, Di Micco R, Genazzani AR, Felsenberg D, Happ J, Hooper MJ, Ittner J, Leb G, Mallmin H, Murray T, Ortolani S, Rubinacci A, Saaf M, Samsioe G, Verbruggen L, Meunier PJ (2002) Intravenous zoledronic acid in postmenopausal women with low bone mineral density. N Engl J Med 346:653–661
Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, Cosman F, Lakatos P, Leung PC, Man Z, Mautalen C, Mesenbrink P, Hu H, Caminis J, Tong K, Rosario-Jansen T, Krasnow J, Hue TF, Sellmeyer D, Eriksen EF, Cummings SR (2007) Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med 356:1809–1822
Lyles KW, Colon-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C, Hyldstrup L, Recknor C, Nordsletten L, Moore KA, Lavecchia C, Zhang J, Mesenbrink P, Hodgson PK, Abrams K, Orloff JJ, Horowitz Z, Eriksen EF, Boonen S (2007) Zoledronic acid and clinical fractures and mortality after hip fracture. New Engl J Med 357:1–11
Black DM, Reid IR, Boonen S, Bucci-Rechtweg C, Cauley JA, Cosman F, Cummings SR, Hue TF, Lippuner K, Lakatos P, Leung PC, Man Z, Martinez RL, Tan M, Ruzycky ME, Su G, Eastell R (2012) The effect of 3 versus 6 years of zoledronic acid treatment of osteoporosis: a randomized extension to the HORIZON-Pivotal Fracture Trial (PFT). J Bone Miner Res 27:243–254 Erratum in: J Bone Miner Res. 2012 Dec;27(12):2612
Black DM, Reid IR, Cauley JA, Cosman F, Leung PC, Lakatos P, Lippuner K, Cummings SR, Hue TF, Mukhopadhyay A, Tan M, Aftring RP, Eastell R (2015) The effect of 6 versus 9 years of zoledronic acid treatment in osteoporosis: a randomized second extension to the HORIZON-Pivotal Fracture Trial (PFT). J Bone Miner Res 30:934–944
Grey A (2016) Intravenous zoledronate for osteoporosis: less might be more. Ther Adv Musculoskelet Dis 8:119–123
Greenspan SL, Perera S, Ferchak MA, Nace DA, Resnick NM (2015) Efficacy and safety of single-dose zoledronic acid for osteoporosis in frail elderly women: a randomized clinical trial. JAMA Intern Med 175:913–921
Tadrous M, Wong L, Mamdani MM, Juurlink DN, Krahn MD, Levesque LE, Cadarette SM (2014) Comparative gastrointestinal safety of bisphosphonates in primary osteoporosis: a network meta-analysis. Osteoporos Int 25:1225–1235
Rizzoli R, Reginster JY, Boonen S, Breart G, Diez-Perez A, Felsenberg D, Kaufman JM, Kanis JA, Cooper C (2011) Adverse reactions and drug-drug interactions in the management of women with postmenopausal osteoporosis. Calcif Tissue Int 89:91–104
Adler RA, El-Hajj Fuleihan G, Bauer DC, Camacho PM, Clarke BL, Clines GA, Compston JE, Drake MT, Edwards BJ, Favus MJ, Greenspan SL, McKinney R Jr, Pignolo RJ, Sellmeyer DE (2016) Managing osteoporosis in patients on long-term bisphosphonate treatment: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 31: 16–35
Khan AA, Morrison A, Kendler DL, Rizzoli R, Hanley DA, Felsenberg D, McCauley LK, O’Ryan F, Reid IR, Ruggiero SL, Taguchi A, Tetradis S, Watts NB, Brandi ML, Peters E, Guise T, Eastell R, Cheung AM, Morin SN, Masri B, Cooper C, Morgan SL, Obermayer-Pietsch B, Langdahl BL, Dabagh RA, Davison KS, Sándor GK, Josse RG, Bhandari M, El Rabbany M, Pierroz DD, Sulimani R, Saunders DP, Brown JP, Compston J (2017) Case-based review of osteonecrosis of the jaw (ONJ) and application of the international recommendations for management from the international task force on ONJ. J Clin Densitom 20:8–24
Fung P, Bedogni G, Bedogni A Petrie A, Porter S, Campisi G, Bagan J, Fusco V, Saia G, Acham S, Musto P, Petrucci MT, Diz P, Colella G, Mignogna MD, Pentenero M, Arduino P, Lodi G, Maiorana C, Manfredi M, Hallberg P, Wadelius M, Takaoka K, Leung YY, Bonacina R, Schiødt M, Lakatos P, Taylor T, De Riu G, Favini G, Rogers SN, Pirmohamed M, Nicoletti P; GENVABO Consortium, Fedele S (2017) Time to onset of bisphosphonate-related osteonecrosis of the jaws: a multicentre retrospective cohort study. Oral Dis 23: 477–483
Meier C, Uebelhart B, Aubry-Rozier B, Birkhäuser M, Bischoff-Ferrari HA, Frey D, Kressig RW, Lamy O, Lippuner K, Stute P, Suhm N, Ferrari S (2017) Osteoporosis drug treatment: duration and management after discontinuation. A position statement from the SVGO/ASCO. Swiss Med Wkly 147:w14484
Rizzoli R, Burlet N, Cahall D, Delmas PD, Eriksen EF, Felsenberg D, Grbic J, Jontell M, Landesberg R, Laslop A, Wollenhaupt M, Papapoulos S, Sezer O, Sprafka M, Reginster JY (2008) Osteonecrosis of the jaw and bisphosphonate treatment for osteoporosis. Bone 42:841–847
Anagnostis P, Paschou SA, Mintziori G, Ceausu I, Depypere H, Lambrinoudaki I, Mueck A, Pérez-López FR, Rees M, Senturk LM, Simoncini T, Stevenson JC, Stute P, Trémollieres FA, Goulis DG (2017) Drug holidays from bisphosphonates and denosumab in postmenopausal osteoporosis: EMAS position statement. Maturitas 101:23–30
Pazianas M, Compston J, Huang CL (2010) Atrial fibrillation and bisphosphonate therapy. J Bone Miner Res 25:2–10
Cardwell CR, Abnet CC, Cantwell MM, Murray LJ (2010) Exposure to oral bisphosphonates and risk of esophageal cancer. JAMA 304:657–663
Green J, Czanner G, Reeves G, Watson J, Wise L, Beral V (2010) Oral bisphosphonates and risk of cancer of oesophagus, stomach, and colorectum: case-control analysis within a UK primary care cohort. BMJ 341:c4444
Shane E, Burr D, Ebeling PR, Abrahamsen B, Adler RA, Brown TD, Cheung AM, Cosman F, Curtis JR, Dell R, Dempster D, Einhorn TA, Genant HK, Geusens P, Klaushofer K, Koval K, Lane JM, McKiernan F, McKinney R, Ng A, Nieves J, O’Keefe R, Papapoulos S, Sen HT, van der Meulen MC, Weinstein RS, Whyte M, American Society for Bone and Mineral Research (2010) Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 25:2267–2294
Rizzoli R, Akesson K, Bouxsein M, Kanis JA, Napoli N, Papapoulos S, Reginster JY, Cooper C (2011) Subtrochanteric fractures after long-term treatment with bisphosphonates: a European Society on Clinical and Economic Aspects of Osteoporosis and Osteoarthritis, and International Osteoporosis Foundation Working Group Report. Osteoporos Int 22:373–390
Meier RP, Perneger TV, Stern R, Rizzoli R, Peter RE (2012) Increasing occurrence of atypical femoral fractures associated with bisphosphonate use. Arch Intern Med 172:930–936
Chlebowski RT, Chen Z, Cauley JA, Anderson G, Rodabough RJ, McTiernan A, Lane DS, Manson JE, Snetselaar L, Yasmeen S, O’Sullivan MJ, Safford M, Hendrix SL, Wallace RB (2010) Oral bisphosphonate use and breast cancer incidence in postmenopausal women. J Clin Oncol 28:3582–3590
Pazianas M, Abrahamsen B, Eiken PA, Eastell R, Russell RG (2012) Reduced colon cancer incidence and mortality in postmenopausal women treated with an oral bisphosphonate-Danish National Register Based Cohort Study. Osteoporos Int 23:2693–2701
Hartle JE, Tang X, Kirchner HL, Bucaloiu ID, Sartorius JA, Pogrebnaya ZV, Akers GA, Carnero GE, Perkins RM (2012) Bisphosphonate therapy, death, and cardiovascular events among female patients with CKD: a retrospective cohort study. Am J Kidney Dis 59:636–644
Bondo L, Eiken P, Abrahamsen B (2013) Analysis of the association between bisphosphonate treatment survival in Danish hip fracture patients-a nationwide register-based open cohort study. Osteoporos Int 24:245–252
Curtis JR, Westfall AO, Cheng H, Delzell E, Saag KG (2008) Risk of hip fracture after bisphosphonate discontinuation: implications for a drug holiday. Osteoporos Int 19:1613–1620
Mignot MA, Taisne N, Legroux I, Cortet B, Paccou J (2017) Bisphosphonate drug holidays in postmenopausal osteoporosis: effect on clinical fracture risk. Osteoporos Int 28:3431–3438
Ensrud KE, Barrett-Connor EL, Schwartz A, Santora AC, Bauer DC, Suryawanshi S, Feldstein A, Haskell WL, Hochberg MC, Torner JC, Lombardi A, Black DM (2004) Randomized trial of effect of alendronate continuation versus discontinuation in women with low BMD: results from the Fracture Intervention Trial long-term extension. J Bone Miner Res 19:1259–1269
Kanis JA, Reginster JY, Kaufman JM, Ringe JD, Adachi JD, Hiligsmann M, Rizzoli R, Cooper C (2012) A reappraisal of generic bisphosphonates in osteoporosis. Osteoporos Int 23:213–221
Kraenzlin ME, Meier C (2011) Parathyroid hormone analogues in the treatment of osteoporosis. Nat Rev Endocrinol 7:647–656
Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, Hodsman AB, Eriksen EF, Ish-Shalom S, Genant HK, Wang O, Mitlak BH (2001) Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med 344:1434–1441
Prince R, Sipos A, Hossain A, Syversen U, Ish-Shalom S, Marcinowska E, Halse J, Lindsay R, Dalsky GP, Mitlak BH (2005) Sustained nonvertebral fragility fracture risk reduction after discontinuation of teriparatide treatment. J Bone Miner Res 20:1507–1513
Vahle JL, Sato M, Long GG, Young JK, Francis PC, Engelhardt JA, Westmore MS, Linda Y, Nold JB (2002) Skeletal changes in rats given daily subcutaneous injections of recombinant human parathyroid hormone (1-34) for 2 years and relevance to human safety. Toxicol Pathol 30:312–321
Jolette J, Wilker CE, Smith SY, Doyle N, Hardisty JF, Metcalfe AJ, Marriott TB, Fox J, Wells DS (2006) Defining a noncarcinogenic dose of recombinant human parathyroid hormone 1-84 in a 2-year study in Fischer 344 rats. Toxicol Pathol 34:929–940
Lecart MP, Reginster JY (2011) Current options for the management of postmenopausal osteoporosis. Expert Opin Pharmacother 12:2533–2552
Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, Delmas P, Zoog HB, Austin M, Wang A, Kutilek S, Adami S, Zanchetta J, Libanati C, Siddhanti S, Christiansen C (2009) Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med 361:756–765
Bone HG, Wagman RB, Brandi ML, Brown JP, Chapurlat R, Cummings SR, Czerwiński E, Fahrleitner-Pammer A, Kendler DL, Lippuner K, Reginster JY, Roux C, Malouf J, Bradley MN, Daizadeh NS, Wang A, Dakin P, Pannacciulli N, Dempster DW, Papapoulos S (2017) 10 years of denosumab treatment in postmenopausal women with osteoporosis: results from the phase 3 randomised FREEDOM trial and open-label extension. Lancet Diabetes Endocrinol 5:513–523
Ferrari S, Adachi JD, Lippuner K, Zapalowski C, Miller PD, Reginster JY, Törring O, Kendler DL, Daizadeh NS, Wang A, O’Malley CD, Wagman RB, Libanati C, Lewiecki EM (2015) Further reductions in nonvertebral fracture rate with long-term denosumab treatment in the FREEDOM open-label extension and influence of hip bone mineral density after 3 years. Osteoporos Int 26:2763–2771
Bone HG, Bolognese MA, Yuen CK, Kendler DL, Miller PD, Yang YC, Grazette L, San Martin J, Gallagher JC (2011) Effects of denosumab treatment and discontinuation on bone mineral density and bone turnover markers in postmenopausal women with low bone mass. J Clin Endocrinol Metab 96:972–980
Cummings SR, Ferrari S, Eastell R, Gilchrist N, Jensen JB, McClung M, Roux C, Törring O, Valter I, Wang AT, Brown JP (2018) Vertebral fractures after discontinuation of denosumab: a post hoc analysis of the randomized placebo-controlled FREEDOM Trial and its extension. J Bone Miner Res 33:190–198
Tsourdi E, Langdahl B, Cohen-Solal M, Aubry-Rozier B, Eriksen EF, Guanabens N, Obermayer-Pietsch B, Ralston SH, Eastell R, Zillikens MC (2017) Discontinuation of denosumab therapy for osteoporosis: a systematic review and position statement by ECTS. Bone 105:11–17
Miller PD, Pannacciulli N, Brown JP, Czerwinski E, Nedergaard BS, Bolognese MA, Malouf J, Bone HG, Reginster JY, Singer A, Wang C, Wagman RB, Cummings SR (2016) Denosumab or zoledronic acid in postmenopausal women with osteoporosis previously treated with oral bisphosphonates. J Clin Endocrinol Metab 101:3163–3170
von Keyserlingk C, Hopkins R, Anastasilakis A, Toulis K, Goeree R, Tarride JE, Xie F (2011) Clinical efficacy and safety of denosumab in postmenopausal women with low bone mineral density and osteoporosis: a meta-analysis. Semin Arthritis Rheum 41:178–186
Black DM, Greenspan SL, Ensrud KE, Palermo L, McGowan JA, Lang TF, Garnero P, Bouxsein ML, Bilezikian JP, Rosen CJ (2003) The effects of parathyroid hormone and alendronate alone or in combination in postmenopausal osteoporosis. N Engl J Med 349:1207–1215
Leder BZ, Tsai JN, Neer RM, Uihlein AV, Wallace PM, Burnett-Bowie SA (2016) Response to therapy with teriparatide, denosumab, or both in postmenopausal women in the DATA (Denosumab and Teriparatide Administration) study randomized controlled trial. J Clin Densitom 19:346–351
Cosman F, Nieves JW, Zion M, Garrett P, Neubort S, Dempster D, Lindsay R (2015) Daily or cyclical teriparatide treatment in women with osteoporosis on no prior therapy and women on alendronate. J Clin Endocrinol Metab 100:2769–2776
Cosman F, Nieves JW, Dempster DW (2017) Treatment sequence matters: anabolic and antiresorptive therapy for osteoporosis. J Bone Miner Res 32:198–202
Kanis JA, Cooper C, Rizzoli R, Reginster J-Y (2018) Review of the guideline of the American College of Physicians on the treatment of osteoporosis. Osteoporos Int 29:1505–1510
Black DM, Bilezikian JP, Ensrud KE, Greenspan SL, Palermo L, Hue T, Lang TF, McGowan JA, Rosen CJ (2005) One year of alendronate after one year of parathyroid hormone (1-84) for osteoporosis. N Engl J Med 353:555–565
Torgerson DJ, Bell-Syer SE (2001) Hormone replacement therapy and prevention of nonvertebral fractures: a meta-analysis of randomized trials. JAMA 285:2891–2897
Cauley JA, Robbins J, Chen Z, Cummings SR, Jackson RD, LaCroix AZ, LeBoff M, Lewis CE, McGowan J, Neuner J, Pettinger M, Stefanick ML, Wactawski-Wende J, Watts NB (2003) Effects of estrogen plus progestin on risk of fracture and bone mineral density: the Women’s Health Initiative randomized trial. JAMA 290:1729–1738
Sornay-Rendu E, Garnero P, Munoz F, Duboeuf F, Delmas PD (2003) Effect of withdrawal of hormone replacement therapy on bone mass and bone turnover: the OFELY study. Bone 33:159–166
Bagger YZ, Tanko LB, Alexandersen P, Hansen HB, Mollgaard A, Ravn P, Qvist P, Kanis JA, Christiansen C (2004) Two to three years of hormone replacement treatment in healthy women have long-term preventive effects on bone mass and osteoporotic fractures: the PERF study. Bone 34:728–735
Roussow JE, Anderson GL, Prentice RL, LaCroix A, Kooperberg C, Stefanick ML (2002) Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA 288:321–333
Wassertheil-Smoller S, Hendrix SL, Limacher M, Heiss G, Kooperberg C, Baird A, Kotchen T, Curb JD, Black H, Rossouw JE, Aragaki A, Safford M, Stein E, Laowattana S, Mysiw WJ (2003) Effect of estrogen plus progestin on stroke in postmenopausal women: the Women’s Health Initiative: a randomized trial. JAMA 289:2673–2684
Chlebowski RT, Hendrix SL, Langer RD, Stefanick ML, Gass M, Lane D, Rodabough RJ, Gilligan MA, Cyr MG, Thomson CA, Khandekar J, Petrovitch H, McTiernan A (2003) Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the Women’s Health Initiative Randomized Trial. JAMA 289:3243–3253
Shumaker SA, Legault C, Rapp SR, Thal L, Wallace RB, Ockene JK, Hendrix SL, Jones BN 3rd, Assaf AR, Jackson RD, Kotchen JM, Wassertheil-Smoller S, Wactawski-Wende J (2003) Estrogen plus progestin and the incidence of dementia and mild cognitive impairment in postmenopausal women: the Women’s Health Initiative Memory Study: a randomized controlled trial. JAMA 289: 2651–2662
Hays J, Ockene JK, Brunner RL, Kotchen JM, Manson JE, Patterson RE, Aragaki AK, Shumaker SA, Brzyski RG, LaCroix AZ, Granek IA, Valanis BG (2003) Effects of estrogen plus progestin on health-related quality of life. N Engl J Med 348:1839–1854
Anderson GL, Limacher M, Assaf AR, Bassford T, Beresford SA, Black H, Bonds D, Brunner R, Brzyski R, Caan B, Chlebowski R, Curb D, Gass M, Hays J, Heiss G, Hendrix S, Howard BV, Hsia J, Hubbell A, Jackson R, Johnson KC, Judd H, Kotchen JM, Kuller L, LaCroix AZ, Lane D, Langer RD, Lasser N, Lewis CE, Manson J, Margolis K, Ockene J, O’Sullivan MJ, Phillips L, Prentice RL, Ritenbaugh C, Robbins J, Rossouw JE, Sarto G, Stefanick ML, Van Horn L, Wactawski-Wende J, Wallace R, Wassertheil-Smoller S (2004) Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA 291: 1701–1712
Fenton A, Panay N (2012) The Women’s Health Initiative—a decade of progress. Climacteric 15:205
Langer RD, Manson JE, Allison MA (2012) Have we come full circle—or moved forward? The Women’s Health Initiative 10 years on. Climacteric 15:206–212
Manson JE, Aragaki AK, Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Chlebowski RT, Howard BV, Thomson CA, Margolis KL, Lewis CE, Stefanick ML, Jackson RD, Johnson KC, Martin LW, Shumaker SA, Espeland MA, Wactawski-Wende J (2017) Menopausal hormone therapy and long-term all-cause and cause-specific mortality: the Women’s Health Initiative randomized trials. JAMA 318:927–938
Langer RD, Simon JA, Pines A, Lobo RA, Hodis HN, Pickar JH, Archer DF, Sarrel PM, Utian WH (2017) Menopausal hormone therapy for primary prevention: why the USPSTF is wrong. Climacteric 20:402–413
Richy F, Ethgen O, Bruyère O, Reginster JY (2004) Efficacy of alphacalcidol and calcitriol in primary and corticosteroid-induced osteoporosis: a meta-analysis of their effects on bone mineral density and fracture rate. Osteoporos Int 15:301–310
Richy F, Schacht E, Bruyère O, Ethgen O, Gourlay M, Reginster JY (2005) Vitamin D analogs versus native vitamin D in preventing bone loss and osteoporosis-related fractures: a comparative meta-analysis. Calcif Tissue Int 76:176–186
Tilyard MW, Spears GF, Thomson J, Dovey S (1992) Treatment of postmenopausal osteoporosis with calcitriol or calcium. N Engl J Med 326:357–362
Gallagher JC, Rapuri PB, Smith LM (2007) An age-related decrease in creatinine clearance is associated with an increase in number of falls in untreated women but not in women receiving calcitriol treatment. J Clin Endocrinol Metab 92:51–58
Shao HB, Yao YM, Wang ZY, Zhang QF, Wei W (2015) Effects of combined alendronate and alfacalcidol on prevention of fractures in osteoporosis patients: a network meta-analysis. Int J Clin Exp Med 8:12935–12941
McCloskey E, Selby P, Davies M, Robinson J, Francis RM, Adams J, Kayan K, Beneton M, Jalava T, Pylkkänen L, Kenraali J, Aropuu S, Kanis JA (2004) Clodronate reduces vertebral fracture risk in women with postmenopausal or secondary osteoporosis: results of a double-blind, placebo-controlled 3-year study. J Bone Miner Res 19:728–736
McCloskey EV, Beneton M, Charlesworth D, Kayan K, deTakats D, Dey A, Orgee J, Ashford R, Forster M, Cliffe J, Kersh L, Brazier J, Nichol J, Aropuu S, Jalava T, Kanis JA (2007) Clodronate reduces the incidence of fractures in community-dwelling elderly women unselected for osteoporosis: results of a double-blind, placebo-controlled randomized study. J Bone Miner Res 22:135–141
Howe J, Huber B, Favell D, Hill R, Bouxsein M, Engelke K, Genant H (2017) Long-term prospective cohort study of a local osteo-enhancement procedure (LOEP) to treat proximal femurs of post-menopausal osteoporotic women. Osteoporos Int 28(S1):S75
Engelke K, Favell D, Hill R, Fuerst T, Huber B, Howe J, Genant H (2017) QCT demonstrates long-term proximal femur trabecular density increases in osteoporotic women following treatment with a minimally invasive local osteo-enhancement procedure involving injection of a resorbable triphasic calcium based implant material. J Bone Miner Res 32(suppl 1):S11
Keaveny T, Lee D, Favell D, Hill R, Howe J, Huber B, Bouxsein M (2017) FEA-estimated proximal femur strength increases through 5-7 year follow-up in osteoporotic women treated with a local osteo-enhancement procedure involving injection of a resorbable, triphasic calcium-based implant material. J Bone Miner Res 32:S11
Boonen S, Van Meirhaeghe J, Bastian L, Cummings SR, Ranstam J, Tillman JB, Eastell R, Talmadge K, Wardlaw D (2011) Balloon kyphoplasty for the treatment of acute vertebral compression fractures: 2-year results from a randomized trial. J Bone Miner Res 26:1627–1637
Wang H, Sribastav SS, Ye F, Yang C, Wang J, Liu H, Zheng Z (2015) Comparison of percutaneous vertebroplasty and balloon kyphoplasty for the treatment of single level vertebral compression fractures: a meta-analysis of the literature. Pain Physician 18:209–222
Papanastassiou ID, Phillips FM, Van Meirhaeghe J, Berenson JR, Andersson GB, Chung G, Small BJ, Aghayev K, Vrionis FD (2012) Comparing effects of kyphoplasty, vertebroplasty, and nonsurgical management in a systematic review of randomized and non-randomized controlled studies. Eur Spine J 21:1826–1843
Firanescu CE, de Vries J, Lodder P, Venmans A, Schoemaker MC, Smeet AJ, Donga E, Juttmann JR, Klazen CAH, Elgersma OEH, Jansen FH, Tielbeek AV, Boukrab I, Schonenberg K, van Rooij WJJ, Hirsch JA, Lohle PNM (2018) Vertebroplasty versus sham procedure for painful acute osteoporotic vertebral compression fractures (VERTOS IV): randomised sham controlled clinical trial. BMJ 360:k1551. https://doi.org/10.1136/bmj.k1551
Beall DP, Tutton SM, Murphy K, Olan W, Warner C, Test JB (2017) Analysis of reporting bias in vertebral augmentation. Pain Physician 20:E1081–E1090
Luthman S, Widén J, Borgström F (2018) Appropriateness criteria for treatment of osteoporotic vertebral compression fractures. Osteoporos Int 29:793–804
Bae JS, Park JH, Kim KJ, Kim HS, Jang IT (2017) Analysis of risk factors for secondary new vertebral compression fracture following percutaneous vertebroplasty in patients with osteoporosis. World Neurosurg 99:387–394
Zhang H, Xu C, Zhang T, Gao Z, Zhang T (2017) Does percutaneous vertebroplasty or balloon kyphoplasty for osteoporotic vertebral compression fractures increase the incidence of new vertebral fractures? A meta-analysis. Pain Physician 20:E13–E28
Chevalley T, Hoffmeyer P, Bonjour JP, Rizzoli R (2002) An osteoporosis clinical pathway for the medical management of patients with low-trauma fracture. Osteoporos Int 13:450–455
McLellan AR, Gallacher SJ, Fraser M, McQuillian C (2003) The fracture liaison service: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporos Int 14:1028–1034
Ganda K, Puech M, Chen JS, Speerin R, Bleasel J, Center JR, Eisman JA, March L, Seibel MJ (2013) Models of care for the secondary prevention of osteoporotic fractures: a systematic review and meta-analysis. Osteoporos Int 24:393–406
Marsh D, Currie C, Brown P et al for the British Orthopaedic Association (2007) The care of patients with fragility fracture. British Orthopaedic Association http://wwwbgsorguk/pdf_cms/pubs/Blue%20Book%20on%20fragility%20fracture%20carepdf Accessed 13 Jan 2018
Akesson K, Marsh D, Mitchell PJ, McLellan AR, Stenmark J, Pierroz DD, Kyer C, Cooper C (2013) Capture the fracture: a best practice framework and global campaign to break the fragility fracture cycle. Osteoporos Int 24:2135–2152
Javaid MK, Kyer C, Mitchell PJ, Chana J, Moss C, Edwards MH, McLellan AR, Stenmark J, Pierroz DD, Schneider MC, Kanis JA, Akesson K, Cooper C (2015) Effective secondary fracture prevention: implementation of a global benchmarking of clinical quality using the IOF capture the fracture (R) best practice framework tool. Osteoporos Int 26:2573–2578
Marsh D, Akesson K, Beaton DE, Bogoch ER, Boonen S, Brandi ML, McLellan AR, Mitchell PJ, Sale JE, Wahl DA (2011) Coordinator-based systems for secondary prevention in fragility fracture patients. Osteoporos Int 22:2051–2065
Davis JC, Guy P, Ashe MC, Liu-Ambrose T, Khan K (2007) HipWatch: osteoporosis investigation and treatment after a hip fracture: a 6-month randomized controlled trial. J Gerontol A Biol Sci Med Sci 62:888–891
Gardner MJ, Flik KR, Mooar P, Lane JM (2002) Improvement in the undertreatment of osteoporosis following hip fracture. J Bone Joint Surg Am 84-A:1342–1348
Majumdar SR, Beaupre LA, Harley CH, Hanley DA, Lier DA, Juby AG, Maksymowych WP, Cinats JG, Bell NR, Morrish DW (2007) Use of a case manager to improve osteoporosis treatment after hip fracture: results of a randomized controlled trial. Arch Intern Med 167:2110–2115
Dell R (2011) Fracture prevention in Kaiser Permanente Southern California. Osteoporos Int 22(Suppl 3):457–460
Majumdar SR, Lier DA, Rowe BH, Russell AS, McAlister FA, Maksymowych WP, Hanley DA, Morrish DW, Johnson JA (2011) Cost-effectiveness of a multifaceted intervention to improve quality of osteoporosis care after wrist fracture. Osteoporos Int 22:1799–1808
Drew S, Judge A, May C, Farmer A, Cooper C, Javaid MK, Gooberman-Hill R (2015) Implementation of secondary fracture prevention services after hip fracture: a qualitative study using extended normalization process theory. Implement Sci 10:57. https://doi.org/10.1186/s13012-015-0243-z
Hawley S, Javaid MK, Prieto-Alhambra D, Lippett J, Sheard S, Arden NK, Cooper C, Judge A (2016) Clinical effectiveness of orthogeriatric and fracture liaison service models of care for hip fracture patients: population-based longitudinal study. Age Ageing 45:236–242
Hawley S, Leal J, Delmestri A, Prieto-Alhambra D, Prieto-Alhambra D, Arden NK, Cooper C, Javaid MK, Judge A (2016) Anti-osteoporosis medication prescriptions and incidence of subsequent fracture among primary hip fracture patients in England and Wales: an interrupted time-series analysis. J Bone Miner Res 31:2008–2015
McLellan AR, Wolowacz SE, Zimovetz EA, Beard SM, Lock S, McCrink L, Adekunle F, Roberts D (2011) Fracture liaison services for the evaluation and management of patients with osteoporotic fracture: a cost-effectiveness evaluation based on data collected over 8 years of service provision. Osteoporos Int 22:2083–2098
Cooper MS, Palmer AJ, Seibel MJ (2012) Cost effectiveness of the Concord minimal trauma Fracture Liaison service, a prospective, controlled fracture prevention study. Osteoporos Int 23:97–107
Leal J, Gray AM, Hawley S, Prieto-Alhambra D, Delmestri A, Arden NK, Cooper C, Javaid MK, Judge A (2017) Cost-effectiveness of orthogeriatric and fracture liaison service models of care for hip fracture patients: a population-based study. J Bone Miner Res 32:203–211
de Bruin IJA, Wyers CE, van den Bergh JPW, Geusens PPMM (2017) Fracture liaison services: do they reduce fracture rates? Ther Adv Musculoskelet Dis 9:157–164
Lekkerkerker F, Kanis JA, Alsayed N, Bouvenot G, Burlet N, Cahall D, Chines A, Delmas P, Dreiser RL, Ethgen D, Hughes N, Kaufman JM, Korte S, Kreutz G, Laslop A, Mitlak B, Rabenda V, Rizzoli R, Santora A, Schimmer R, Tsouderos Y, Viethel P, Reginster JY (2007) Adherence to treatment of osteoporosis: a need for study. Osteoporos Int 18:1311–1317
Solomon DH, Avorn J, Katz JN, Finkelstein JS, Arnold M, Polinski JM, Brookhart MA (2005) Compliance with osteoporosis medications. Arch Intern Med 165:2414–2419
Rabenda V, Mertens R, Fabri V, Vanoverloop J, Sumkay F, Vannecke C, Deswaef A, Verpooten GA, Reginster JY (2008) Adherence to bisphosphonates therapy and hip fracture risk in osteoporotic women. Osteoporos Int 19:811–818
Hiligsmann M, Gathon HJ, Bruyère O, Ethgen O, Rabenda V, Reginster JY (2010) Cost-effectiveness of osteoporosis screening followed by treatment: the impact of medication adherence. Value Health 13:394–401
Ross S, Samuels E, Gairy K, Iqbal S, Badamgarav E, Siris E (2011) A meta-analysis of osteoporotic fracture risk with medication nonadherence. Value Health 14:571–581
Strom O, Borgstrom F, Kanis JA, Jonsson B (2009) Incorporating adherence into health economic modelling of osteoporosis. Osteoporos Int 20:23–34
Kanis JA, Cooper C, Hiligsmann M, Rabenda V, Reginster JY, Rizzoli R (2011) Partial adherence: a new perspective on health economic assessment in osteoporosis. Osteoporos Int 22:2565–2573
Caro JJ, Ishak KJ, Huybrechts KF, Raggio G, Naujoks C (2004) The impact of compliance with osteoporosis therapy on fracture rates in actual practice. Osteoporos Int 15:1003–1008
Rabenda V, Reginster JY (2010) Overcoming problems with adherence to osteoporosis medication. Expert Rev Pharmacoecon Outcomes Res 10:677–689
Hiligsmann M, Bours SP, Boonen A (2015) A review of patient preferences for osteoporosis drug treatment. Curr Rheumatol Rep 17(9):61. https://doi.org/10.1007/s11926-015-0533-0
Iglay K, Cao X, Mavros P, Joshi K, Yu S, Tunceli K (2015) Systematic literature review and meta-analysis of medication adherence with once-weekly versus once-daily therapy. Clin Ther 37:1813–1821
Diez-Perez A, Naylor KE, Abrahamsen B, Agnusdei D, Brandi ML, Cooper C, Dennison E, Eriksen EF, Gold DT, Guañabens N, Hadji P, Hiligsmann M, Horne R, Josse R, Kanis JA, Obermayer-Pietsch B, Prieto-Alhambra D, Reginster JY, Rizzoli R, Silverman S, Zillikens MC, Eastell R (2017) International Osteoporosis Foundation and European Calcified Tissue Society Working Group. Recommendations for the screening of adherence to oral bisphosphonates. Osteoporos Int 28:767–774
Carr AJ, Thompson PW, Cooper C (2006) Factors associated with adherence and persistence to bisphosphonate therapy in osteoporosis: a cross-sectional survey. Osteoporos Int 17:1638–1644
Rabenda V, Bruyère O, Reginster JY (2011) Relationship between bone mineral density changes and risk of fractures among patients receiving calcium with or without vitamin D supplementation: a meta-regression. Osteoporos Int 22:893–901
Hochberg MC, Greenspan S, Wasnich RD, Miller P, Thompson DE, Ross PD (2002) Changes in bone density and turnover explain the reductions in incidence of nonvertebral fractures that occur during treatment with antiresorptive agents. J Clin Endocrinol Metab 87:1586–1592
Delmas PD, Li Z, Cooper C (2004) Relationship between changes in bone mineral density and fracture risk reduction with antiresorptive drugs: some issues with meta-analyses. J Bone Miner Res 19:330–337
Cummings SR, Karpf DB, Harris F, Genant HK, Ensrud K, LaCroix AZ, Black DM (2002) Improvement in spine bone density and reduction in risk of vertebral fractures during treatment with antiresorptive drugs. Am J Med 112:281–289
Watts NB, Geusens P, Barton IP, Felsenberg D (2005) Relationship between changes in BMD and nonvertebral fracture incidence associated with risedronate: reduction in risk of nonvertebral fracture is not related to change in BMD. J Bone Miner Res 20:2097–2104
Sarkar S, Mitlak BH, Wong M, Stock JL, Black DM, Harper KD (2002) Relationships between bone mineral density and incident vertebral fracture risk with raloxifene therapy. J Bone Miner Res 17:1–10
Austin M, Yang YC, Vittinghoff E, Adami S, Boonen S, Bauer DC, Bianchi G, Bolognese MA, Christiansen C, Eastell R, Grauer A, Hawkins F, Kendler DL, Oliveri B, McClung MR, Reid IR, Siris ES, Zanchetta J, Zerbini CA, Libanati C, Cummings SR (2012) Relationship between bone mineral density changes with denosumab treatment and risk reduction for vertebral and nonvertebral fractures. J Bone Miner Res 27:687–693
Chen P, Miller PD, Delmas PD, Misurski DA, Krege JH (2006) Change in lumbar spine BMD and vertebral fracture risk reduction in teriparatide-treated postmenopausal women with osteoporosis. J Bone Miner Res 21:1785–1790
Baim S, Wilson CR, Lewiecki EM, Luckey MM, Downs RW Jr, Lentle BC (2005) Precision assessment and radiation safety for dual-energy X-ray absorptiometry: position paper of the International Society for Clinical Densitometry. J Clin Densitom 8: 371–378
Bjarnason NH, Sarkar S, Duong T, Mitlak B, Delmas PD, Christiansen C (2001) Six and twelve month changes in bone turnover are related to reduction in vertebral fracture risk during 3 years of raloxifene treatment in postmenopausal osteoporosis. Osteoporos Int 12:922–930
Eastell R, Christiansen C, Grauer A, Kutilek S, Libanati C, McClung MR, Reid IR, Resch H, Siris E, Uebelhart D, Wang A, Weryha G, Cummings SR (2011) Effects of denosumab on bone turnover markers in postmenopausal osteoporosis. J Bone Miner Res 26:530–537
Diez-Perez A, Adachi JD, Agnusdei D, Bilezikian JP, Compston JE, Cummings SR, Eastell R, Eriksen EF, Gonzalez-Macias J, Liberman UA, Wahl DA, Seeman E, Kanis JA, Cooper C for the IOF CSA Inadequate Responders Working Group (2012) Treatment failure in osteoporosis. Osteoporos Int 23:2769–2774
Marseille E, Larson B, Kazi DS, Kahn JG Rosen S (2015) Thresholds for the cost-effectiveness of interventions: alternative approaches. Bull WHO 93:118–124
Gyrd-Hansen D (2006) Looking for willingness to pay (wtp) threshold for a qaly—does it make sense? A critical view. The International Society For Pharmacoeconomics And Outcomes Research (ISPOR). https://www.ispor.org/news/articles/July07/WTP-CW.asp Accessed 18 February 2018
Kanis JA, Jonsson B (2002) Economic evaluation of interventions for osteoporosis. Osteoporos Int 13:765–767
National Institute for Health and Care Excellence (2011) NICE technology appraisal guidance 161 (amended). Alendronate, etidronate, risedronate, raloxifene, strontium ranelate and teriparatide for the secondary prevention of osteoporotic fragility fractures in postmenopausal women (amended). In: NICE London
Nimdet K, Chaiyakunapruk N, Vichansavakul K, Ngorsuraches S (2015) A systematic review of studies eliciting willingness-to-pay per quality-adjusted life year: does it justify CE threshold? PLoS One 10(4):e0122760. https://doi.org/10.1371/journal.pone.0122760
Hiligsmann M, Evers SM, Sedrine WB, Kanis JA, Ramaekers B, Reginster JY, Silverman S, Wyers CE, Boonen A (2015) A systematic review of cost-effectiveness analyses of drugs for postmenopausal osteoporosis. Pharmacoeconomics 33:205–224
National Institute for Health and Care Excellence (2011b) NICE technology appraisal guidance 160 (amended). Alendronate, etidronate, risedronate, raloxifene and strontium ranelate for the primary prevention of osteoporotic fragility fractures in postmenopausal women (amended). NICE London
Kanis JA, McCloskey E, Jonsson B, Cooper C, Strom B, Borgstrom F (2010) An evaluation of the NICE guidance for the prevention of osteoporotic fragility fractures in postmenopausal women. Arch Osteoporos 5:19–48
Hiligsmann M, Kanis JA, Compston J, Cooper C, Flamion B, Bergmann P, Body JJ, Boonen S, Bruyère O, Devogelaer JP, Goemaere S, Kaufman JM, Rozenberg S, Reginster JY (2013) Health technology assessment in osteoporosis. Calcif Tissue Int 93:1–14
Kanis JA, Hiligsmann M (2014) The application of health technology assessment in osteoporosis. Best Pract Res Clin Endocrinol Metab 28:895–910
Brandão CM, Machado GP, Acurcio F (2012) Pharmacoeconomic analysis of strategies to treat postmenopausal osteoporosis: a systematic review. Rev Bras Reumatol 52:924–937
Strom O, Borgstrom F, Sen SS, Boonen S, Haentjens P, Johnell O, Kanis JA (2007) Cost-effectiveness of alendronate in the treatment of postmenopausal women in 9 European countries--an economic evaluation based on the fracture intervention trial. Osteoporos Int 18:1047–1061
Borgstrom F, Johnell O, Kanis JA, Jonsson B, Rehnberg C (2006) At what hip fracture risk is it cost-effective to treat? International intervention thresholds for the treatment of osteoporosis. Osteoporos Int 17:1459–1471
Lippuner K, Johansson H, Borgstrom F, Kanis JA, Rizzoli R (2012) Cost-effective intervention thresholds against osteoporotic fractures based on FRAX(R) in Switzerland. Osteoporos Int 23:2579–2589
Makras P, Athanasakis K, Boubouchairopoulou N, Rizou S, Anastasilakis AD, Kyriopoulos J, Lyritis GP (2015) Cost-effective osteoporosis treatment thresholds in Greece. Osteoporos Int 26:1949–1957
Marques A, Lourenço O, Ortsäter G, Borgström F, Kanis JA, da Silva JAP (2016) Cost-effectiveness of osteoporosis treatment intervention thresholds for the treatment of osteoporosis based on FRAX in Portugal. Calcif Tissue Intl 99: 131–141
Harvey NC, McCloskey E, Kanis JA, Compston J, Cooper C (2017) Bisphosphonates in osteoporosis: NICE and easy? Lancet 390(10109):2243–2244. https://doi.org/10.1016/S0140-6736(17)32850-7
McCloskey EV, Johansson H, Odén A, Vasireddy S, Kayan K, Pande K, Jalava T, Kanis JA (2009) Ten-year fracture probability identifies women who will benefit from clodronate therapy--additional results from a double-blind, placebo-controlled randomised study. Osteoporos Int 20:811–817
Harvey NC, Kanis JA, Odén A, Burge RT, Mitlak BH, Johansson H, McCloskey EV (2015) FRAX and the effect of teriparatide on vertebral and non-vertebral fracture. Osteoporos Int 26:2347–2353
Harvey NC, Kanis JA, Odén A, Nakamura T, Shiraki M, Sugimoto T, Kuroda T, Johansson H, McCloskey EV (2015b) Efficacy of weekly teriparatide does not vary by baseline fracture probability calculated using FRAX. Osteoporos Int 26:2347–2354
McCloskey EV, Johansson H, Odén A, Austin M, Siris E, Wang A, Lewiecki EM, Lorenc R, Libanati C, Kanis JA (2012) Denosumab reduces the risk of all osteoporotic fractures in postmenopausal women, particularly in those with moderate to high fracture risk as assessed with FRAX®. J Bone Miner Res 27:1480–1486
Donaldson MG, Palermo L, Ensrud KE, Hochberg MC, Schousboe JT, Cummings SR (2012) Effect of alendronate for reducing fracture by FRAX score and femoral neck bone mineral density: the Fracture Intervention Trial. J Bone Miner Res 27:1804–1810
Kim K, Svedbom A, Luo X, Sutradhar S, Kanis JA (2014) Comparative cost-effectiveness of bazedoxifene and raloxifene in the treatment of postmenopausal osteoporosis in Europe using the FRAX algorithm. Osteoporos Int 25:325–337
Hiligsmann M, Ben Sedrine W, Reginster JY (2013) Cost-effectiveness of bazedoxifene compared with raloxifene in the treatment of postmenopausal osteoporotic women. J Bone Miner Res 28(4):807–815
Kendler DL, Marin F, Zerbini CAF, Russo LA, Greenspan SL, Zikan V, Bagur A, Malouf-Sierra J, Lakatos P, Fahrleitner-Pammer A, Lespessailles E, Minisola S, Body JJ, Geusens P, Möricke R, López-Romero P (2017) Effects of teriparatide and risedronate on new fractures in post-menopausal women with severe osteoporosis (VERO): a multicentre, double-blind, double-dummy, randomised controlled trial. Lancet pii: S0140-6736(17)32137–32132. https://doi.org/10.1016/S0140-6736(17)32137-2
Acknowledgements
We are grateful to the IOF Committee of Scientific Advisors and the Committee of National Societies to the ESCEO Scientific Advisory Board for their review of this paper and its endorsement. The paper updates the earlier guidance of 2013 [3] ‘European guidance for the diagnosis and management of osteoporosis in postmenopausal women’ and many sections of text are reproduced with kind permission of from Springer Science and Business Media B.V. The summary and recommendations are in close accord with those established by the UK National Osteoporosis Guideline Group [85] of which JAK and CC are members.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interests
JAK reports grants from Amgen, Eli Lilly and Radius Health; non-financial support from Medimaps, and Asahi; and other support from AgNovos. JAK is the architect of FRAX® but has no financial interest. CC reports personal fees from Alliance for Better Bone Health, Amgen, Eli Lilly, GSK, Medtronic, Merck, Novartis, Pfizer, Roche, Servier, Takeda and UCB. RR has received consulting fees or advisory board fees from Radius Health, Labatec, Danone, Nestlé, CNIEL and Sandoz. J-YR has received advisory board or consulting fees from IBSA-Genévrier, Pierre Fabre, Radius Health, TEVA and Mylan; and lecture fees from Anovos, IBSA-Genévrier, Mylan, CNIEL, Dairy Research Council (DRC) and Theramex; and institutional grant support from IBSA-Genévrier, Mylan, CNIEL and Radius Health.
Additional information
The original version of this article was revised due to a retrospective Open Access order.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kanis, J., Cooper, C., Rizzoli, R. et al. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 30, 3–44 (2019). https://doi.org/10.1007/s00198-018-4704-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-018-4704-5