Abstract
Summary
We analyzed women and newborn outcome after maternal exposure to BPs. BPs have no teratogenic effect on the 36 analyzed pregnancies compared to unexposed controls matched on women underlying diseases (either systemic disease, either “bone” disease) but some outcome differed: neonatal complications rate in systemic diseases and live birth rate in bone diseases).
Introduction
The effect of bisphosphonates (BPs) during pregnancy remains unclear. We aimed to study pregnancy outcomes in women exposed to BPs during pregnancy.
Methods
Data for cases and controls were from the French Reference Centre of Teratogenic Agents. Cases were women who received BPs in the 6 weeks before or during a pregnancy and had systemic or bone diseases. We included two respectively matched control groups: women with systemic diseases not exposed to BPs and healthy women not exposed to BPs or any teratogenic agent. Four controls were assigned to each case.
Results
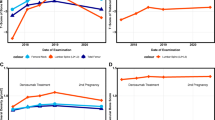
Thirty-six women were exposed to BPs including 5 just before pregnancy and 30 during the first trimester; 23 had systemic diseases (systemic lupus erythematosus, n = 5; rheumatoid arthritis, n = 5; other, n = 13) and 13 had bone diseases. Rate of observed congenital malformations did not differ in women with a systemic or a bone disease compared to their respective controls (respectively 2/23 [8.7%] vs 2/92 [2.2%], p = 0.178 and 0/13 [0%] vs 0/52 [0%], p = 1.00). Among women with systemic diseases, non-specific neonatal complications were more frequent for cases (4/16 [25.0%] vs 4/64 [6.3%], p = 0.027). Among women with bone disorders, the live birth rate was lower for cases than healthy controls (8/10 [80%] vs 50/50 [100%], p = 0.025).
Conclusion
We found no major teratogenic effects of BPs, but rates of neonatal complications were increased for women with systemic diseases, as were spontaneous abortions for women with bone diseases likely linked to the severity of the underlying diseases and concomitant medications.
Similar content being viewed by others
References
Minisola S, Pepe J, Piemonte S, Cipriani C (2015) The diagnosis and management of hypercalcaemia. BMJ 350:h2723
Rizzoli R, Biver E (2014) Glucocorticoid-induced osteoporosis: who to treat with what agent? Nat Rev Rheumatol 11(2):98–109
Grossman JM, Gordon R, Ranganath VK, Deal C, Caplan L, Chen W, Curtis JR, Furst DE, McMahon M, Patkar NM, Volkmann E, Saag KG (2010) American College of Rheumatology 2010 recommendations for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Care Res 62(11):1515–1526
Mäkitie AA, Törnwall J, Mäkitie O (2008) Bisphosphonate treatment in craniofacial fibrous dysplasia—a case report and review of the literature. Clin Rheumatol 27(6):809–812
Drake MT, Clarke BL, Khosla S (2008) Bisphosphonates: mechanism of action and role in clinical practice. In: Mayo Clinic proceedings. Elsevier, pp 1032–1045
Lin JH, Duggan DE, Chen I-W, Ellsworth RL (1991) Physiological disposition of alendronate, a potent anti-osteolytic bisphosphonate, in laboratory animals. Drug Metab Dispos 19(5):926–932
Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, Cosman F, Lakatos P, Leung PC, Man Z, Mautalen C, Mesenbrink P, Hu H, Caminis J, Tong K, Rosario-Jansen T, Krasnow J, Hue TF, Sellmeyer D, Eriksen EF, Cummings SR, HORIZON Pivotal Fracture Trial (2007) Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med 356(18):1809–1822
Khan SA, Kanis JA, Vasikaran S, Kline WF, Matuszewski BK, McCloskey EV, Beneton MNC, Gertz BJ, Sciberras DG, Holland SD, Orgee J, Coombes GM, Rogers SR, Porras AG (1997) Elimination and biochemical responses to intravenous alendronate in postmenopausal osteoporosis. J Bone Miner Res 12(10):1700–1707
Papapoulos SE, Cremers SCLM (2007) Prolonged bisphosphonate release after treatment in children. N Engl J Med 356(10):1075–1076
Patlas N, Golomb G, Yaffe P, Pinto T, Breuer E, Ornoy A (1999) Transplacental effects of bisphosphonates on fetal skeletal ossification and mineralization in rats. Teratology 60(2):68–73
McKenzie AF, Budd RS, Yang C, Shapiro B, Hicks RJ (1994) Technetium-99m-methylene diphosphonate uptake in the fetal skeleton at 30 weeks gestation. J Nucl Med 35(8):1338–1341
Okazaki A, Matsuzawa T, Takeda M et al (1995) Intravenous reproductive and developmental toxicity studies of cimadronate (YM175), a novel bisphosphonate, in rats and rabbits. J Toxicol Sci 20(SupplementI):1–13
Minsker DH, Manson JM, Peter CP (1993) Effects of the bisphosphonate, alendronate, on parturition in the rat. Toxicol Appl Pharmacol 121(2):217–223
Levy S, Fayez I, Taguchi N, Han JY, Aiello J, Matsui D, Moretti M, Koren G, Ito S (2009) Pregnancy outcome following in utero exposure to bisphosphonates. Bone 44(3):428–430
Ornoy A, Wajnberg R, Diav-Citrin O (2006 Nov) The outcome of pregnancy following pre-pregnancy or early pregnancy alendronate treatment. Reprod Toxicol 22(4):578–579
Ioannis SP, Chrysoula LG, Aikaterini K, George T, George LP, Nikolaos PA, Symeon T (2011) The use of bisphosphonates in women prior to or during pregnancy and lactation. Hormones 10(4):280–291
Boocock GR, Todd PJ (1985) Inguinal hernias are common in preterm infants. Arch Dis Child 60(7):669–670
Wroblewska-Seniuk K, Chojnacka K, Pucher B, Szczapa J, Gadzinowski J, Grzegorowski M (2005) The results of newborn hearing screening by means of transient evoked otoacoustic emissions. Int J Pediatr Otorhinolaryngol 69(10):1351–1357
J Vettukattil J (2016) Pathophysiology of patent ductus arteriosus in the preterm infant. Curr Pediatr Rev 12(2):120–122
Perez-Aytes A, Marin-Reina P, Boso V, Ledo A, Carey JC, Vento M (2017) Mycophenolate mofetil embryopathy: a newly recognized teratogenic syndrome. Eur J Med Genet 60(1):16–21
Delabaere A, Huchon C, Deffieux X, Beucher G, Gallot V, Nedellec S, Vialard F, Carcopino X, Quibel T, Subtil D, Barasinski C, Gallot D, Vendittelli F, Laurichesse-Delmas H, Lémery D (2014) Epidemiology of loss pregnancy. J Gynecol Obstet Biol Reprod (Paris) 43(10):764–775
Losada I, Sartori L, Di Gianantonio E, Zen M, Clementi M, Doria A (2010) Bisphosphonates in patients with autoimmune rheumatic diseases: can they be used in women of childbearing age? Autoimmun Rev 9(8):547–552
Munns CF, Rauch F, Ward L, Glorieux FH (2004) Maternal and fetal outcome after long-term pamidronate treatment before conception: a report of two cases. J Bone Miner Res 19(10):1742–1745
Castillo H, Samson-Fang L (2009) Effects of bisphosphonates in children with osteogenesis imperfecta: an AACPDM systematic review. Dev Med Child Neurol 51(1):17–29
Chan B, Zacharin M (2006) Maternal and infant outcome after pamidronate treatment of polyostotic fibrous dysplasia and osteogenesis imperfecta before conception: a report of four cases. J Clin Endocrinol Metab 91(6):2017–2020
Hassen-Zrour S, Korbaa W, Béjia I, Saidani Z, Bergaoui N (2010) Maternal and fetal outcome after long-term bisphosphonate exposure before conception. Osteoporos Int 21(4):709–710
Dunlop DJ, Soukop M, McEwan HP (1990) Antenatal administration of aminopropylidene diphosphonate. Ann Rheum Dis 49(11):955
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Aurélien Sokal, Tifenn Leturcq, Delphine Beghin, and Xavier Mariette declare that they have no conflict of interest.
Raphaele Seror received consulting fees from Roche and Novartis.
Rights and permissions
About this article
Cite this article
Sokal, A., Elefant, E., Leturcq, T. et al. Pregnancy and newborn outcomes after exposure to bisphosphonates: a case-control study. Osteoporos Int 30, 221–229 (2019). https://doi.org/10.1007/s00198-018-4672-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-018-4672-9