Abstract
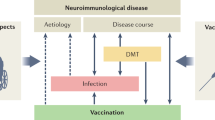
The spectrum of inflammatory diseases of the central nervous system has been steadily expanding from classical autoimmune disorders such as multiple sclerosis to far more diverse diseases. Evidence now suggests that syndromes such as Alzheimer's disease and stroke have important inflammatory and immune components and may be amenable to treatment by anti-inflammatory and immunotherapeutic approaches. The notion of 'vaccinating' individuals against a neurodegenerative disorder such as Alzheimer's disease is a marked departure from classical thinking about mechanism and treatment, and yet therapeutic vaccines for both Alzheimer's disease and multiple sclerosis have been validated in animal models and are in the clinic. Such approaches, however, have the potential to induce unwanted inflammatory responses as well as to provide benefit.
Similar content being viewed by others
Main
Inflammation of the central nervous system (CNS) may be the result of both innate and adaptive immune responses. In Alzheimer's disease (AD) an innate immune response is triggered by local production of amyloid β-protein (Aβ), whereas in multiple sclerosis (MS) an adaptive immune response directed against myelin components initiates inflammation in the CNS (Table 1). Adaptive immune responses involving antibody- or cell-mediated responses have differential effects in AD and MS, and in animal models of these diseases. In addition, the recent appearance of encephalitis in individuals with AD that have been immunized with Aβ has parallels to underlying mechanisms of cell-mediated adaptive immune responses in MS, in which pro-inflammatory T-cell responses seem to drive the disease. These features of inflammation, which are outlined for AD and MS in Table 1, are reviewed here in terms of both disease pathogenesis and therapy.
Multiple sclerosis
Multiple sclerosis is an inflammatory disease of the central nervous system characterized by perivascular cuffs of mononuclear cells that include both lymphocytes and macrophages1. This infiltration leads to damage of the myelin sheath and the underlying axon. Activation of microglia and astrocytes occurs in MS, but it is secondary to infiltrating lymphocytes. In the initial stages of the disease, the inflammation that occurs in MS is episodic and associated with discrete attacks of neurological dysfunction followed by recovery, which may leave residual neurological damage. Subsequently the disease often becomes more progressive, developing to a stage where there is less inflammation and nervous system damage is caused by a degenerative process initiated by the inflammation.
The episodic inflammation that is classic of MS is clearly visualized by magnetic resonance imaging (MRI) scans of the brain after administration of the contrast material gadolinium2. Gadolinium crosses an open blood–brain barrier created by the inflammation and highlights discrete areas of inflammation. The duration of enhanced inflammation in individuals receiving weekly MRI scans is 4–8 weeks, and virtually all new lesions enhance in their earliest phases3. When the acute inflammation resolves, it leaves a scar and tissue damage. This can be seen in the three-dimensional MRI images in Fig. 1, which were recorded over a 1-yr period in a single individual affected with MS. The new inflammatory focus can be seen appearing adjacent to the ventricle and then beginning to resolve. The inflammatory process of MS is associated with a complex cascade of inflammatory molecules and mediators, including chemokines, adhesion molecules associated with activated endothelial cell walls and matrix metalloproteases4,5,6.
The cause of the recurrent inflammation in MS is now generally accepted to be autoimmune in nature, that is, a cell-mediated autoimmune attack against the white matter sheath7. An alternative explanation for the episodic and chronic inflammation that is the hallmark of MS is the presence of a virus or infectious agent that has persistently infected the nervous system. But although infectious agents have been extensively sought in MS, none has been isolated8. Viruses and infectious agents are, however, thought to be important in triggering the immune system and the immune attack on the nervous system9. Given the inflammatory nature of the pathological process and the autoimmune hypothesis, one might expect that anti-inflammatory immunosuppressive drugs would reduce inflammation, as measured by MRI imaging, and positively affect the clinical course. Indeed, this has been shown clearly with agents such as mitoxanthrone10, a chemotherapy drug, and cyclophosphamide11,12, a chemotherapy drug that is also used in other inflammatory conditions such as lupus nephritis and inflammatory muscle disease. The most widely used drugs in MS, β-interferon and glatiramer acetate, have anti-inflammatory and immunomodulatory effects and are discussed in more detail below13.
Adaptive cell-mediated immune responses in MS
The adaptive immune system can be classified broadly into cellular and humoral (antibody)-type responses. Among cellular responses, different types or classes of cellular immune responses have been identified that are essential to understanding the mechanisms of the inflammatory process in MS and to devising strategies to control it. As discussed below, the different classes of cell-mediated immune response have important implications for attempts to develop a vaccination strategy not only for MS but also for AD.
Cellular immune responses can be classified as TH1-type or TH2-type responses (Fig. 2), depending on how they differentiate from TH0 precursors14. TH1 (or pro-inflammatory) responses are induced when T cells differentiate in the presence of interleukin 12 (IL-12), and TH1 cells are characterized by the secretion of interferon-γ (IFN-γ) and inflammatory mediators such as tumour-necrosis factor-α (TNF-α). TH1-type responses are important in fighting viral infections, and MS seems to be a cell-mediated autoimmune disease of a TH1 type. Anti-inflammatory T-cell responses include both TH2 responses and T cells that have been classified as 'regulatory cells'. TH2 responses are induced when T cells differentiate in the presence of IL-4, and TH2-type cells secrete anti-inflammatory cytokines such as IL-4 and IL-10. TH2-type responses are important in fighting parasitic infections, and TH1 and TH2 responses may cross-regulate each other.
a, Multiple sclerosis is thought to be induced by the generation of TH1-type myelin-reactive cells from precursor cells (THP), which are presumed to be triggered by crossreactive antigens such as viruses in the context of co-stimulatory molecules and IL-12. TH1-type cells directed against myelin migrate into the nervous system where they re-encounter myelin antigens presented by microglia and are restimulated to initiate a destructive inflammatory cascade. Immune therapy involves the induction of anti-inflammatory regulatory T cells (TH2, TH3, TR1, CD25+ cells) that secrete anti-inflammatory cytokines, such as IL-4, IL-10 and TGF-β, or may also act by cell to cell contact (CD25+ cells). These regulatory cells inhibit TH1 responses in the periphery and/or migrate to the CNS, where they are re-stimulated by local microglia cells and inhibit or suppress the local inflammatory cascade in the CNS. Regulatory cells can be induced by different means, including glatiramer acetate (Copaxone), altered peptide ligands, mucosal administration of antigen and compounds that block co-stimulation pathways33,37,41.
Another class of T cell comprises regulatory cells that can downregulate TH1-type inflammatory processes. Different types of regulatory cell have been described15. TH3 cells act primarily through the secretion of transforming growth factor-β (TGF-β) and are preferentially induced at mucosal surfaces16, TR1 cells (T regulatory cell 1) act primarily through the secretion of IL-10 (ref. 17), and CD4+CD25+ regulatory cells are T cells that express CD25 (IL-2 receptor) and exert potent regulatory function through cell contact and also through cytokines such as IL-10 and TGF-β (ref. 18). If MS is a TH1-type cell-mediated autoimmune disease, it might be possible to regulate the TH1 responses by the induction of regulatory cell populations.
The induction of TH1-type myelin-reactive cells and their migration into the nervous system is shown in Fig. 2a. It is postulated that THP (T precursor) myelin-reactive T cells are induced to differentiate into myelin-reactive TH1 cells when an antigen that crossreacts with a myelin antigen is presented to a T cell by an antigen-presenting cell in the context of IL-12 and co-stimulatory molecules. It is generally thought that viruses with structures that crossreact with myelin antigens act as crossreactive antigens19. TH1 T cells that react with myelin antigens, such as proteolipid protein (PLP), myelin basic protein (MBP) and myelin oligodendrocyte glycoprotein (MOG), cross the blood–brain barrier where the myelin antigens are represented to the T cell by antigen-presenting cells in the brain (microglia cells), and an inflammatory cascade is triggered with the release of inflammatory mediators that cause damage to the myelin sheath and ultimately the underlying axon.
One of the primary animal models for MS, experimental allergic encephalomyelitis (EAE), is induced by immunizing different mouse or rat strains with a myelin autoantigen (such as MBP, PLP or MOG) given in complete Freund's adjuvant, which induces a TH1-type cell-mediated response against the myelin antigen. In EAE, myelin-reactive TH1-type CD4+ T cells migrate from the periphery into the CNS, where they also initiate a cascade of immune-mediated damage (Fig. 2a). In animals, EAE can be induced by the adoptive transfer of TH1-type CD4+ cells specific for one of the myelin proteins.
The hypothesis that MS is a inflammatory TH1-type disease is supported by several observations. First, it has been shown directly by the effects of β-interferon, the prototypic TH1 cytokine, which when administered to individuals with MS caused clinical exacerbations20. Second, individuals affected with MS have a TH1 bias, as indicated by increased concentrations of IL-12 (refs 21, 22) and IL-18 (ref. 23), both of which induce IFN-γ and increase TH1-type chemokine receptor expression5,24. Last, IL-12-secreting cells in the peripheral blood are linked to inflammation in the CNS, as measured by gadolinium enhancement on MRI imaging25: increased numbers of IL-12-secreting cells in the blood are associated with gadolinium enhancement, and cyclophosphamide decreases the number of IL-12-secreting cells, which is linked to clinical response26.
In addition to IL-12, it has been shown recently that osteopontin is important in TH1 differentiation in autoimmune demyelinating disease27,28. The most widely used immunomodulatory drug in MS, β-interferon, seems to have two broad mechanisms of action: it decreases γ-interferon secretion by cells in the peripheral blood and blocks the migration of T cells across the blood–brain barrier13.
Vaccination
The term 'vaccination' stems from the original observation of Jenner and his use of subcutaneous administration of cowpox to prevent the subsequent development of smallpox. Since then, the term vaccination has acquired a broader meaning. According to current immunological theory, vaccination is no longer restricted to administering infectious agents but applies to manipulating the immune system in a manner that regulates or suppresses inflammatory and even non-inflammatory processes that can cause tissue damage. Thus, one can redefine vaccination as 'the generation or induction of an immune response that is beneficial to the host in halting a pathological process', irrespective of whether that process is immune-mediated, autoimmune or even inflammatory.
Thus, vaccination involves not only the use of the immune system itself to correct or to alter abnormal immune responses that cause damage, but the immune system may be used to affect beneficially pathological processes that are neither autoimmune nor inflammatory. A striking example is represented by reports of the effectiveness of active immunization with Aβ peptide in adjuvant29 and the passive administration of antibodies against Aβ30 to clear amyloid deposits and their surrounding glia and neuronal cytopathology from the brains of transgenic mouse models of AD.
It has also become clear that injury to the nervous system by non-immune mechanisms, such as stroke or trauma, may have a secondary stage associated with inflammation and that immune-based therapies can decrease CNS damage. For example, oral administration of MBP in a rat model of stroke decreases infarct size after middle cerebral artery occlusion and this is associated with increased expression of the anti-inflammatory cytokine TGF-β in the nervous system31, and nasal administration of myelin oligodendrocyte glycoprotein (MOG) has similar effects in a mouse model of stroke (D. Frenkel and H.W., unpublished results). In an extensive series of studies, Schwartz and co-workers32 have shown that T-cell autoimmunity against myelin antigens can be beneficial in animal models of central nervous system trauma caused by crush injury of the optic nerve or spinal cord contusion. Thus, an 'inflammatory response' directed against nervous system tissue also has the potential to have a protective or beneficial role.
Antigen-specific vaccination in MS
Antigen-specific modulation of the immune system is presumed to be the most specific and potentially least toxic way in which to manipulate the immune system in disease and represents the classic model of vaccination, that is, the induction of an antigen-specific beneficial immune response. For MS, a TH1-type cell-mediated disease, the strategy is to induce TH2 or antigen-specific regulatory cells (Table 1 and Fig. 2b).
Numerous approaches using antigen-specific therapy have been successful in the murine EAE model and some of these have been tested in individuals with MS. The most successful so far has been the use of glatiramer acetate or copolymer 1, which is now an approved therapy for MS13. Glatiramer acetate is a random copolymer of four amino acids that was designed to mimic MBP and thus to induce EAE. It does not have encephalitogenic properties but instead works effectively in what seems to be an antigen-specific manner to suppress EAE by generating regulatory T cells. Although glatiramer acetate has several effects on the immune system, it seems principally to be acting as an altered peptide ligand that induces TH2- and TH3-type regulatory cells, which react in the CNS to suppress inflammation33.
One of the major conceptual conundrums in designing antigen-specific vaccines for MS relates to the issue of which antigen to administer in MS. There is reactivity to several myelin antigens in MS34,35, both because MS seems to be a syndrome rather than a single disease and because of epitope spreading, in which damage caused by a T cell specific for one myelin antigen induces reactivity to another myelin antigen36. This conundrum seems to have been resolved by the phenomenon of bystander suppression, in which antigen-specific myelin-reactive regulatory cells are induced that secrete anti-inflammatory cytokines such as IL-10 and TGF-β (ref. 37). Such regulatory cells secrete anti-inflammatory cytokines when they encounter the autoantigen in the target tissue and thus suppress inflammation in the CNS caused by T cells of a different specificity. Thus, in the EAE model, one can suppress PLP-induced EAE by glatiramer acetate, by mucosal administration of MBP or by the use of altered peptide ligands of MBP, all of which induce anti-inflammatory regulatory T-cell responses (TH2, TH3). Of note, in immune-deficient mice, TH2-type responses can induce a form of EAE38.
But therapeutic vaccination is not without potential risks both in MS and in AD. In the early 1980s, Jonas Salk and colleagues attempted to treat individuals with MS by injecting large amounts of MBP subcutaneously to 'vaccinate' against putative harmful T-cell responses to MBP. They could induce both cellular and humoral (antibody) immune responses to MBP but obtained no consistent positive clinical effects and even some suggestion that the injections might have been harmful39. To obviate harmful sensitization by injection of MBP, an analogous approach was undertaken using an altered peptide ligand of MBP in which key amino acid sequences had been altered so that injection caused a TH2 or TH3 response as opposed to a TH1 response. Results of a phase II trial showed that injections of large doses of the peptide led to a worsening of MS inflammation in some people, as measured by gadolinium-enhanced lesions on brain MRI, and an increased number of cells reactive to MBP40. As part of a larger trial in individuals given a smaller dose, however, positive effects were observed on MRI and immune deviation towards TH2-type responses was observed41.
As discussed below, an Aβ vaccine developed for use in AD has been found to cause adverse effects, which were most probably related to the induction of TH1-type T-cell responses against Aβ. Of note, T-cell vaccination with myelin-reactive T cells to downregulate pathogenic TH1 responses has been applied successfully to the EAE model and is being tested in individuals with MS28,42,43,44, but it is not applicable to AD because there is no evidence of a pathogenic adaptive T-cell response in AD. DNA vaccination is another approach for treating CNS autoimmune diseases such as MS and has been used effectively in the EAE model by several investigators45,46,47,48.
Alzheimer's disease
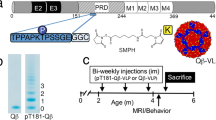
Alzheimer's disease is the most common form of age-related cognitive failure in humans. It is characterized neuropathologically by the progressive accumulation of the 42-residue Aβ peptide in limbic and association cortices, where some of it precipitates to form a range of amorphous and compacted extracellular plaques49. These plaques, particularly the more compacted ones, are associated with dystrophic neurites (altered axons and dendrites), activated microglia and reactive astrocytes. Some of these dystrophic neurites contain intracellular bundles of abnormal paired helical filaments composed of insoluble, hyperphosphorylated forms of the microtubule-associated protein, tau. Paired helical filaments also accumulate in large cytoplasmic masses, called neurofibrillary tangles, in the cell bodies of innumerable limbic and neocortical neurons. The detection of neuritic (amyloid) plaques and neurofibrillary tangles in brain regions important for memory and other cognitive functions provides the basis for confirming a clinical diagnosis of AD after death.
Although it has become increasingly recognized that inflammation may be important in the neuropathological damage that occurs in AD, unlike MS the inflammation in AD seems to arise from inside the CNS with little or no involvement of lymphocytes or monocytes beyond their normal surveillance of the brain50,51,52. The inflammatory cytopathology (microgliosis, astrocytosis, complement activation, increased cytokine expression and acute phase protein response) is thought to represent a secondary response to the early accumulation of Aβ in the brain (Fig. 3). This innate immune response that occurs in the brain, which is presumably secondary to amyloid deposition, leads to the accumulation of inflammatory mediators such as TNF-α, IL-1, IL-6, free radicals and microglia activation.
Accumulation of Aβ leads to stimulation of the innate immune response, including activation of microglia and astrocytes, release of cytokines such as TNF-α and IL-β, complement activation and free-radical formation. This innate immune activation may contribute to neurotoxicity. An adaptive immune response induced by vaccination with Aβ generates antibodies against Aβ; these antibodies decrease accumulation of Aβ in the brain through Fc-mediated clearance and also seem to draw Aβ from the brain into the cerebrospinal fluid and to the bloodstream. The adaptive immune response is under T-cell control and, depending on genetic background and T-cell immune tolerance, the effectiveness of vaccination to induce antibodies may be enhanced or decreased. In the context of Aβ vaccination and as part of the adaptive immune response, TH1-type T cells directed against Aβ may be induced, which migrate to the nervous system and which may trigger an inflammatory response and a clinical picture of meningoencephalitis.
To what degree this activation of microglia53,54 and other potential antigen-presenting CNS cells and secretors of cytokines is involved in the progressive neurodegenerative process is not yet clear, although it has been generally assumed to do more harm than good. Studies of transgenic mice that overexpress an AD-causing mutant form of human amyloid precursor protein (APP) and develop amyloid deposits have shown, however, that crossing such mice with mice overexpressing a natural inhibitor of complement C3 results in a worsening of Aβ plaque load and more neuronal loss55. This result suggests that the inflammatory changes found in AD and mouse models thereof, including activation of the classical complement cascade, may represent a beneficial response, at least in part. Nonetheless, clinical studies suggest that conventional anti-inflammatory drugs such as those used in arthritis may delay or slow the progression of AD50.
Despite the fact that only local innate inflammation occurs in AD, the theory and immune mechanisms of therapeutic vaccination discussed above with reference to MS have unexpectedly become relevant to AD, because the induction of specific adaptive immune responses has been shown to be of benefit in the animal model of AD (Fig. 3). It has been discovered that parenteral immunization of APP transgenic mice with synthetic Aβ in complete Freund's adjuvant can markedly decrease the number and density of Aβ deposits in the brain, with concomitant improvements in neuritic dystrophy and gliosis29. Positive effects have also been found after repetitive mucosal (intranasal) administration of the peptide to transgenic mice56. It seems that the induction of antibodies against Aβ has a primary role in the vaccine-mediated clearance of Aβ from the brain, because passive transfer of Aβ antibodies has shown similar beneficial neuropathological effects30. Notably, a single parenteral administration of a monoclonal antibody against Aβ has been shown to produce rapid (within hours) benefits on certain behavioural measures of cognitive function in a mouse model, apparently by interfering with some diffusible, putatively synaptotoxic form of Aβ (for example, Aβ oligomers) without lowering the overall amount of Aβ deposits in the brain57.
Two broad theories about the mechanisms by which Aβ antibodies work in mice have emerged. First, evidence of Fc-mediated uptake and clearance of Aβ antibody complexes by local activated microglia has been obtained30. Second, evidence of a net movement of Aβ peptide out of the brain as a result of its binding and mobilization by Aβ antibodies, both peripherally (in the serum) and centrally (in the cerebrospinal fluid), has been provided58. These two proposed mechanisms are not mutually exclusive, and there may be additional ways in which antibodies decrease Aβ-mediated synaptic and neuronal dysfunction. So far there is no clear evidence that T cells have either a protective or an injurious effect in AD or its mouse models, but this possibility needs further research. As discussed below, T-cell responses seem to have a role in the generation of meningoencephalitis after Aβ vaccination to induce antibodies.
Human trials of Aβ vaccination in AD
The finding that active vaccination with Aβ could profoundly reduce quantities of Aβ peptide in an animal model led to early clinical trials in which an Aβ1–42 synthetic peptide was administered parenterally with a previously tested adjuvant (QS21) to individuals with mild to moderate AD. Although a phase I safety study in few individuals did not detect significant side-effects, a subsequent phase II trial was discontinued shortly after its initiation when roughly 5% of the treated participants developed what seemed to be an inflammatory reaction in the CNS (an aseptic meningoencephalitis). The occurrence of the meningocerebral inflammation was not correlated with either the presence or titres of antibodies against Aβ among the trial participants59. The mechanism of this self-limited inflammatory reaction is unknown, but the appearance of the inflammation before the detection of Aβ antibodies in some of the recipients may suggest that a T-cell-mediated immune reaction to Aβ was responsible. Such cellular reactions were not detected in mice and other mammals exposed to the vaccine during preclinical safety and efficacy testing, although a recent report suggests autoimmune encephalomyelitis can be induced in mice vaccinated with Aβ peptide plus pertussis60.
Efforts are underway to determine the basis for the adverse inflammatory reaction induced by Aβ1–42 and to attempt to model it in animals. No abnormal effects have been documented in APP transgenic mouse models to which Aβ antibodies have been administered, and such mice have shown robust clearing of brain Aβ deposits and even improvements in behavioural deficits30,57. This is in contrast to the EAE model in which administration of antibody to MOG worsens the progression of EAE61. There is therefore an interest in conducting trials with a humanized monoclonal antibody to Aβ as the next step in the clinical evaluation of the immunotherapeutic approach to AD. It may also be possible to immunize with portions of Aβ to generate only antibodies that target N-terminal residues62,63.
Aβ as an autoantigen
We have found recently that APP transgenic mice, which produce robust quantities of Aβ in the brain, have a form of immunological tolerance in which they show significantly lower T-cell responses when immunized with Aβ than do wild-type mice63. This deficit can be overcome in part by providing T-cell help to the animal. Thus, the presence of abundant Aβ in the brain may not only cause local neuronal and glia damage but also hinder the generation of a therapeutic immune response, whether innate or induced.
Very recently, we have begun to extend such analyses to humans and, by using sensitive short-term cloning techniques, have found heightened in vitro reactivity of peripheral T-cells against Aβ in some elderly individuals and people with AD64. Early studies did not find lymphocyte proliferation in response to APP peptides in individuals with AD65. The likelihood of seeing this T-cell hypereactivity in humans increased with age but was not observed in all individuals with AD or all aged normal individuals. Our results raise the possibility that endogenous T-cell reactivity in a host may relate to the progression of the cytopathological process of AD. In addition, such data suggest that it may useful to test individuals for their intrinsic T-cell reactivity to Aβ before offering them any immunotherapeutic based on Aβ.
Beneficial versus deleterious T-cell responses
The issue of beneficial versus deleterious T-cell responses in vaccination models against CNS antigens is a concept that applies to approaches in both AD and MS. It has been shown that deleterious T-cell responses, presumably related to the induction of TH1-type responses, can be induced in humans affected with either AD or MS. This does not mean that vaccination approaches in CNS diseases cannot be successful, as has been shown by the use of glatiramer acetate in MS; however, strategies that induce nonpathogenic T-cell responses must be utilized, for example, modified autoantigens, tolerogenic routes such as mucosal administration and non-TH1-inducing adjuvants should be used, and careful attention should be paid to dosing. In addition, the genetic background of the host and the immune repertoire may also determine whether a detrimental T-cell response will occur after vaccination.
For example, we have found that SJL mice strains immunized with MOG peptide in complete Freund's adjuvant are susceptible to EAE, whereas B10S mice treated similarly are resistant66. This does not seem to relate to the generation of immune response against MOG, but to the type of immune response. In the SJL mouse there is infiltration of cells expressing γ-interferon in the brain and a predominantly TH1 response, whereas in the B10S mice there is a TH2 and TH3 response that seems to prevent disease. Thus, the immune repertoire of the host before vaccination may determine the outcome of vaccination.
It seems that vaccination strategies both in AD and in MS will be dependent on skewing the immune response in such a way that it is not harmful to the host. In this regard, we have found in the APP mouse model of AD that nasal administration of Aβ induces antibody responses in association with an 'anti-inflammatory' cellular immune response involving IL-4, IL-10 and TGF-β56. These 'anti-inflammatory' responses may themselves help the pathologic process by suppressing inflammation and microglial activation, which are believed to contribute to the CNS dysfunction in AD50,51,52. Furthermore, cells secreting TGF-β may themselves aid in the clearance of Aβ67. Such Aβ-reactive T cells would act in the CNS only at sites where Aβ is involved in the inflammatory process and thus would not be expected to interfere with normal physiology.
References
Prineas, J. W. in Handbook of Multiple Sclerosis (ed. Cook, S. D.) 223–255 (Marcel Dekker, Newark NJ, 1996).
Miller, D. H., Grossman, R. I., Reingold, S. C. & McFarland, H. F. The role of magnetic resonance techniques in understanding and managing multiple sclerosis. Brain 121, 3–24 (1998).
Weiner, H. L. et al. Serial magnetic resonance imaging in multiple sclerosis: correlation with attacks, disability, and disease stage. J. Neuroimmunol. 104, 164–173 (2000).
Cannella, B. & Raine, C. S. The adhesion molecule and cytokine profile of multiple sclerosis lesions. Ann. Neurol. 37, 424–435 (1995).
Sorensen, T. L. et al. Expression of specific chemokines and chemokine receptors in the central nervous system of multiple sclerosis patients. J. Clin. Invest. 103, 807–815 (1999).
Cuzner, M. L. et al. The expression of tissue-type plasminogen activator, matrix metalloproteases and endogenous inhibitors in the central nervous system in multiple sclerosis: comparison of stages in lesion evolution. J. Neuropathol. Exp. Neurol. 55, 1194–1204 (1996).
Weiner, H. L. A 21 point unifying hypothesis on the etiology and treatment of multiple sclerosis. Can. J. Neurolog. Sci. 25, 93–101 (1998).
Cook, S. D., Rohowsky-Kochan, C., Bansil, S. & Dowling, P. C. in Handbook of Multiple Sclerosis (ed. Cook, S. D.) 97–118 (Marcel Dekker, Newark, NJ, 1996).
Sibley, W. A., Bamford, C. R. & Clark, K. Clinical viral infections and multiple sclerosis. Lancet 1, 1313–1315 (1985).
Edan, G. et al. Therapeutic effect of mitoxantrone combined with methylprednisolone in multiple sclerosis: a randomised multicenter study of active disease using MRI and clinical criteria. J. Neurol. Neurosurg. Psychiat. 62, 112–118 (1997).
Gobbini, M. I., Smith, M. E., Richert, N. D., Frank, J. A. & McFarland, H. F. Effect of open label pulse cyclophosphamide therapy on MRI measures of disease activity in five patients with refractory relapsing-remitting multiple sclerosis. J. Neuroimmunol. 99, 142–149 (1999).
Weiner, H. L. & Cohen, J. A. Treatment of multiple sclerosis with cyclophosphamide: critical review of clinical and immunologic effects. Mult. Scler. 8, 142–154 (2002).
Goodin, D. S. et al. Disease modifying therapies in multiple sclerosis: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and the MS Council for Clinical Practice Guidelines. Neurology 58, 169–178 (2002).
Mosmann, T. R. & Sad, S. The expanding universe of T-cell subsets: Th1, Th2, and more. Immunol. Today 17, 138–146 (1996).
Maloy, K. J. & Powrie, F. Regulatory T cells in the control of immune pathology. Nature Immunol. 2, 816–822 (2001).
Weiner, H. L. Induction and mechanism of action of transforming growth factor-β-secreting Th3 regulatory cells. Immunol. Rev. 182, 207–214 (2001).
Groux, H. et al. A CD4+ T-cell subset inhibits antigen-specific T-cell responses and prevents colitis. Nature 389, 737–742 (1997).
Sakaguchi, S., Sakaguchi, N., Asano, M., Itoh, M. & Toda, M. Immunologic self-tolerance maintained by activated T cells expressing IL-2 receptor α-chains (CD25). Breakdown of a single mechanism of self-tolerance causes various autoimmune diseases. J. Immunol. 155, 1151–1164. (1995).
Wucherpfennig, K. W. & Strominger, J. L. Molecular mimicry in T cell-mediated autoimmunity: viral peptides activate human T cell clones specific for myelin basic protein. Cell 80, 695–705 (1995).
Panitch, H. S., Hirsch, R. L., Haley, A. S. & Johnson, K. P. Exacerbations of multiple sclerosis in patients treated with gamma interferon. Lancet 1, 893–895 (1987).
Balashov, K. E., Smith, D. R., Khoury, S. J., Hafler, D. A. & Weiner, H. L. Increased IL-12 production in progressive multiple sclerosis: induction by activated CD4+ T-cells via CD40 ligand. Proc. Natl Acad. Sci. USA 94, 599–603 (1997).
Windhagen, A. et al. Expression of costimulatory molecules B7-1 (CD80), B7-2 (CD86), and interleukin 12 cytokine in multiple sclerosis lesions. J. Exp. Med. 182, 1985–1996 (1995).
Karni, A., Koldzic, D. N., Bharanidharan, P., Khoury, S. J. & Weiner, H. L. IL-18 is linked to raised IFN-γ in multiple sclerosis and is induced by activated CD4+ T cells via CD40–CD40 ligand interactions. J. Neuroimmunol. 125, 134–140 (2002).
Balashov, K. E., Rottman, J. B., Weiner, H. L. & Hancock, W. W. CCR5+ and CXCR3+ T cells are increased in multiple sclerosis and their ligands MIP-1α and IP-10 are expressed in demyelinating brain lesions. Proc. Natl Acad. Sci. USA 96, 6873–6878 (1999).
Makhlouf, K., Weiner, H. L. & Khoury, S. J. Increased percentage of IL-12+ monocytes in the blood correlates with the presence of active MRI lesions in MS. J. Neuroimmunol. 119, 145–149 (2001).
Comabella, M. et al. Elevated interleukin-12 in progressive multiple sclerosis correlates with disease activity and is normalized by pulse cyclophosphamide therapy. J. Clin. Invest. 102, 671–678 (1998).
Chabas, D. et al. The influence of the proinflammatory cytokine, osteopontin, on autoimmune demyelinating disease. Science 294, 1731–1735 (2001).
Jansson, M., Panoutsakopoulou, V., Baker, J., Klein, L. & Cantor, H. Cutting edge: attenuated experimental autoimmune encephalomyelitis in eta-1/osteopontin-deficient mice. J. Immunol. 168, 2096–2099 (2002).
Schenk, D. et al. Immunization with amyloid-β attenuates Alzheimer-disease-like pathology in the PDAPP mouse. Nature 400, 173–177 (1999).
Bard, F. et al. Peripherally administered antibodies against amyloid β-peptide enter the central nervous system and reduce pathology in a mouse model of Alzheimer disease. Nature Med. 6, 916–919 (2000).
Becker, K. J. et al. Immunologic tolerance to myelin basic protein decreases stroke size after transient focal cerebral ischemia. Proc. Natl Acad. Sci. USA 94, 10873–10878 (1997).
Moalem, G. et al. Autoimmune T cells protect neurons from secondary degeneration after central nervous system axotomy. Nature Med. 5, 49–55 (1999).
Neuhaus, O., Farina, C., Wekerle, H. & Hohlfeld, R. Mechanisms of action of glatiramer acetate in multiple sclerosis. Neurology 56, 702–708 (2001).
Olsson, T. et al. Autoreactive T lymphocytes in multiple sclerosis determined by antigen-induced secretion of interferon-γ. J. Clin. Invest. 86, 981–985 (1990).
Zhang, J. et al. Increased frequency of IL-2 responsive T-cells specific for myelin basic protein and proteolipid protein in peripheral blood and cerebrospinal fluid of patients with multiple sclerosis. J. Exp. Med. 179, 973–984 (1993).
Lehmann, P., Forsthuber, T., Miller, A. & Sercarz, E. Spreading of T-cell autoimmunity to cryptic determinants of an autoantigen. Nature 358, 155–157 (1992).
Miller, A., Lider, O. & Weiner, H. L. Antigen-driven bystander suppression following oral administration of antigens. J. Exp. Med. 174, 791–798 (1991).
Lafaille, J. J. et al. Myelin basic protein-specific T helper 2 (Th2) cells cause experimental autoimmune encephalomyelitis in immunodeficient hosts rather than protect them from the disease. J. Exp. Med. 186, 307–312 (1997).
Romine, J. S. & Salk, J. in Multiple Sclerosis: Pathology, Diagnosis and Management (eds Hallpike, J. F., Adams, C. M. W. & Tourtelotte, W. W.) 621–630 (Williams & Wilkins, Baltimore, 1983).
Bielekova, B. et al. Encephalitogenic potential of the myelin basic protein peptide (amino acids 83–99) in multiple sclerosis: results of a phase II clinical trial with an altered peptide ligand. Nature Med. 6, 1167–1175 (2000).
Kappos, L. et al. Induction of a non-encephalitogenic type 2 T helper-cell autoimmune response in multiple sclerosis after administration of an altered peptide ligand in a placebo-controlled, randomized phase II trial. The Altered Peptide Ligand in Relapsing MS Study Group. Nature Med. 6, 1176–1182 (2000).
Kumar, V., Sercarz, E., Zhang, J. & Cohen, I. T-cell vaccination: from basics to the clinic. Trends Immunol. 22, 539–540 (2001).
Vandenbark, A. A. et al. TCR peptide therapy in human autoimmune diseases. Neurochem. Res. 26, 713–730 (2001).
Medaer, R., Stinissen, P., Truyen, L., Raus, J. & Zhang, J. Depletion of myelin-basic-protein autoreactive T cells by T-cell vaccination: pilot trial in multiple sclerosis. Lancet 346, 807–808 (1995).
Weissert, R. et al. Protective DNA vaccination against organ-specific autoimmunity is highly specific and discriminates between single amino acid substitutions in the peptide autoantigen. Proc. Natl Acad. Sci. USA 97, 1689–1694 (2000).
Wildbaum, G., Westermann, J., Maor, G. & Karin, N. A targeted DNA vaccine encoding fas ligand defines its dual role in the regulation of experimental autoimmune encephalomyelitis. J. Clin. Invest. 106, 671–679 (2000).
Wildbaum, G., Netzer, N. & Karin, N. Plasmid DNA encoding IFN-γ-inducible protein 10 redirects antigen-specific T cell polarization and suppresses experimental autoimmune encephalomyelitis. J. Immunol. 168, 5885–5892 (2002).
Garren, H. et al. Combination of gene delivery and DNA vaccination to protect from and reverse Th1 autoimmune disease via deviation to the Th2 pathway. Immunity 15, 15–22 (2001).
Selkoe, D. J. Alzheimer's disease: genes, proteins and therapies. Physiol. Rev. 81, 742–761 (2001).
Akiyama, H. et al. Inflammation and Alzheimer's disease. Neurobiol. Aging 21, 383–421 (2000).
Cooper, N. R., Kalaria, R. N., McGeer, P. L. & Rogers, J. Key issues in Alzheimer's disease inflammation. Neurobiol. Aging 21, 451–453 (2000).
McGeer, E. G. & McGeer, P. L. The importance of inflammatory mechanisms in Alzheimer disease. Exp. Gerontol. 33, 371–378 (1998).
El Khoury, J., Hickman, S. E., Thomas, C. A., Loike, J. D. & Silverstein, S. C. Microglia, scavenger receptors, and the pathogenesis of Alzheimer's disease. Neurobiol. Aging 19, S81–S84 (1998).
Meda, L. et al. Activation of microglial cells by β-amyloid protein and interferon-γ. Nature 374, 647–650 (1995).
Wyss-Coray, T. et al. Prominent neurodegeneration and increased plaque formation in complement-inhibited Alzheimer's mice. Proc. Natl Acad. Sci. USA 99, 10837–10842 (2002).
Weiner, H. L. et al. Nasal administration of amyloid-β peptide decreases cerebral amyloid burden in mouse model of Alzheimer's disease. Ann. Neurol. 48, 567–579 (2000).
Dodart, J. C. et al. Immunization reverses memory deficits without reducing brain Aβ burden in Alzheimer's disease model. Nature Neurosci. 5, 452–457 (2002).
DeMattos, R. B. et al. Peripheral anti-Aβ antibody alters CNS and plasma Aβ clearance and decreases brain Aβ burden in a mouse model of Alzheimer's disease. Proc. Natl Acad. Sci. USA 98, 8850–8855 (2001).
Schenk, D. in Immunization against Alzheimer's Disease and Other Neurodegenerative Disorders (eds Selkoe, D. & Christen, Y.) (Springer, Heidelberg, in the press).
Furlan, R. et al. Vaccination with amyloid-β peptide induces autoimmune encephalomyelitis in C57BL/6 mice. Brain (in the press).
Linington, C., Engelhardt, B., Kapocs, G. & Lassman, H. Induction of persistently demyelinated lesions in the rat following the repeated adoptive transfer of encephalitogenic T cells and demyelinating antibody. J. Neuroimmunol. 40, 219–224 (1992).
McLaurin, J. et al. Therapeutically effective antibodies against amyloid-β peptide target amyloid-β residues 4–10 and inhibit cytotoxicity and fibrillogenesis. Nature Med. 11, 1263–1269 (2002).
Monsonego, A., Maron, R., Zota, V., Selkoe, D. J. & Weiner, H. L. Immune hyporesponsiveness to amyloid β-peptide in amyloid precursor protein transgenic mice: implications for the pathogenesis and treatment of Alzheimer's disease. Proc. Natl Acad. Sci. USA 98, 10273–10278 (2001).
Monsonego, A. et al. Immunogenic aspects of amyloid β-peptide: implications for pathogenesis and treatment of Alzheimer's disease. Abstr. no. 423 in Proc. VIII Int. Conf. on Alzheimer's Disease and Related Disorders, Stockholm, Sweden (2002).
Trieb, K., Ransmayr, G., Sgonc, R., Lassmann, H. & Grubeck-Loebenstein, B. APP peptides stimulate lymphocyte proliferation in normals, but not in patients with Alzheimer's disease. Neurobiol. Aging 17, 541–547 (1996).
Maron, R. et al. Genetic susceptibility or resistance to autoimmune encephalomyelitis in MHC congenic mice is associated with differential production of pro- and anti-inflammatory cytokines. Int. Immunol. 11, 1573–1580 (1999).
Wyss-Coray, T. et al. TGF-β1 promotes microglial amyloid-beta clearance and reduces plaque burden in transgenic mice. Nature Med. 7, 612–618 (2001).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Weiner, H., Selkoe, D. Inflammation and therapeutic vaccination in CNS diseases. Nature 420, 879–884 (2002). https://doi.org/10.1038/nature01325
Issue Date:
DOI: https://doi.org/10.1038/nature01325
This article is cited by
-
METTL3 Mediates Microglial Activation and Blood–Brain Barrier Permeability in Cerebral Ischemic Stroke by Regulating NLRP3 Inflammasomes Through m6A Methylation Modification
Neurotoxicity Research (2024)
-
Arsenic trioxide ameliorates experimental autoimmune encephalomyelitis in C57BL/6 mice by inducing CD4+ T cell apoptosis
Journal of Neuroinflammation (2020)
-
Modulatory Effects of Nicotine on neuroHIV/neuroAIDS
Journal of Neuroimmune Pharmacology (2018)
-
An advanced white matter tract analysis in frontotemporal dementia and early-onset Alzheimer’s disease
Brain Imaging and Behavior (2016)
-
Dynamics of the meningeal CD4+ T-cell repertoire are defined by the cervical lymph nodes and facilitate cognitive task performance in mice
Molecular Psychiatry (2014)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.