Abstract
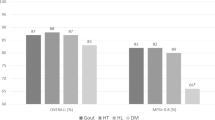
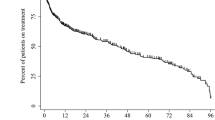
To identify adherence and persistence levels with urate-lowering therapies using the national administrative pharmacy claim database. This was a retrospective, pharmacy claims-based analysis of dispensed anti-gout medications on the Irish national HSE-PCRS scheme database between January 2008 and December 2012. Adherence is defined by the medication possession ratio (MPR), and patients were considered to be adherent if the MPR ≥80 % (good adherers) in any given time period. Persistence was defined as continued use of therapy with no periods exceeding a refill gap of >63 days (9 weeks). Logistic regression analysis was used to predict odd ratios (OR) and 95 % confidence interval (CI) for persistence and adherence in relation to age, gender and level of comorbidity. There was a 53 % increase in the number of patients prescribed anti-gout medications between 2008 and 2012 with an increase of 27 % in the associated ingredient cost of these medications. Allopurinol accounted for 87 % of the prescribing and febuxostat accounted for a further 9 %. In patients who started on 100 mg allopurinol, only 14.6 % were titrated to the 300 mg dose. For all those initiating urate-lowering therapies, 45.8 % of patients were persistent with treatment at 6 months decreasing to 22.6 % at 12 months. In multivariate analysis, females had poorer adherence (OR = 0.83 (0.77–0.90)), and increasing age was associated with increased adherence (OR = 4.19 (2.53–6.15)) Increasing comorbidity score was associated with increased adherence and persistence at 6 months (OR = 0.68 (0.59–0.79)). Adherence with anti-gout medications in this study cohort was relatively low. Sustained treatment for gouty arthritis is essential in the prevention of serious adverse outcomes.
Significance and Innovations
–Poor adherence to medications prescribed to patients for the management of chronic diseases such as gout is an ongoing problem which urgently needs to be addressed.
–Some of the reasons identified for poor adherence to anti-gout medications include the risk of flare of acute gout with the initiation of urate-lowering therapy (ULT), poor response to ULT and persistence of attacks of acute gout, suboptimal dosing of allopurinol therapy and intolerance of allopurinol.
–The results of this study identified adherence and persistence rates of approximately 50 % at 6 months which is in line if not lower than many of the other published studies to date which have measured adherence and persistence using pharmacy claims databases.
–The results of poor adherence and persistence affect both the health of the patients with financial implications for the healthcare service.


Similar content being viewed by others
References
Rott KT, Agudelo CA (2003) Gout. JAMA 289:2857–2860
Shoji A, Yamanaska H, Kamatani N (2004) A retrospective study of the relationship between serum urate level and recurrent attacks of gouty arthritis: evidence for reduction of recurrent gouty arthritis with antihyperuricemic therapy. Arthritis Rheum 51(3):321–325
Roddy E, Doherty M (2010) Epidemiology of Gout. Arthritis Res Ther 12:223
Arthritis Ireland: http://www.arthritisireland.ie/go/information/frequently_asked_questions. (Accessed: August 13th 2013)
Harrold LR, Andrade SE (2009) Medication adherence of patients with selected rheumatic conditions: a systematic review of the literature. Semin Arthritis Rheum 38:396–402
de Klerk E, van der Heijde D, Landewe R, van der Tempel H, Urquhart J, van der Linden S (2003) Patients compliance in rheumatoid arthritis, polymyalgia rheumatic, and gout. J Rheumatol 30:44–54
Zhang W, Doherty M, Bardin T, Pascual E, Barskova V, Conaghan P, Gerster J, Jacobs J, Leeb B, Lioté F, McCarthy G, Netter P, Nuki G, Perez-Ruiz F, Pignone A, Pimentão J, Punzi L, Roddy E, Uhlig T, Zimmermann-Gòrska I (2006) EULAR Standing Committee for International Clinical Studies Including Therapeutics. EULAR evidence based recommendations for gout. Part II: management. Report of a task force of the EULAR standing committee for international clinical studies including therapeutics. Ann Rheum Dis 65(10):1312–1324
Hande KR, Noone RM, Stone WJ (1984) Severe allopurinol toxicity. Description and guidelines for prevention in patients with renal insufficiency. Am J Med 76(1):47–56
Stamp LK, O'Donnell JL, Zhang M, James J, Frampton C, Barclay ML, Chapman PT (2011) Using allopurinol above the dose based on creatinine clearance is effective and safe in patients with chronic gout, including those with renal impairment. Arthritis Rheum 63(2):412–421
Dalbeth N, House ME, Horne A, Petrie KJ, McQueen FM, Taylor WJ (2012) Prescription and dosing of urate-lowering therapy, rather than patient behaviours, are the key modifiable factors associated with targeting serum urate in gout. BMC Musculoskelet Disord 13:174
HSE-Primary Care Reimbursement Service Statistical Analysis of Claims and Payments 2011. http://www.hse.ie/eng/staff/PCRS/PCRS_Publications/pcrsclaimsandpayments2011.pdf Accessed September 22nd 2013
WHO anatomical therapeutic chemical classification. Oslo: WHO, 2013. http://www.whocc.no/atc_ddd_index/ Accessed: May 10th 2013
Andrade SE, Kahler KH, Frech F, Chan KA (2006) Methods for evaluation of medication adherence and persistence using automateddatabases. Pharmacoepidemiol Drug Saf 15:565–574
Sloan KL, Sales AE, Liu CF, Nichol P, Suzuki NT, Sharp ND (2003) Construction and characteristics of the RxRisk V: A VA adapted pharmacy based case –mix instrument. Med Care 41(6):761–774
O'Shea MP, Teeling M, Bennett K (2013) An observational study examining the effect of co morbidity on the rates of persistence and adherence to newly initiated oral anti-hyperglycaemic agents. Pharmacoepidemiol Drug Saf. doi:10.1002/pds.3535
Roddy E, Zhang W, Doherty M (2007) The changing epidemiology of gout. Nat Clin Pract Rheumatol 3:443–449
Wallace KL, Riedel AA, Joseph-Ridge N, Wortmann R (2004) Increasing prevalence of gout and hyperuricemia over 10 years among older adults in a managed care population. J Rheumatol 31:1582–1587
Lawrence RC, Helmick CG, Arnett FC et al (1998) Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum 41:778–799
Helmick CG, Felson DT, Lawrence RC et al (2008) Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part I. Arthritis Rheum 58:15–25
Lawrence RC, Felson DT, Helmick CG et al (2008) Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum 58:26–35
Arromdee E, Michet CJ, Crowson CS, O'Fallon WM, Gabriel SE (2002) Epidemiology of gout: is the incidence rising? J Rheumatol 29:2403–2406
Harris CM, Lloyd DC, Lewis J (1995) The prevalence and prophylaxis of gout in England. J Clin Epidemiol 48:1153–1158
Mikuls TR, Farrar JT, Bilker WB, Fernandes S, Schumacher HR Jr, Saag KG (2005) Gout epidemiology: results from the UK general practice research database, 1990–1999. Ann Rheum Dis 64:267–272
Annemans L, Spaepen E, Gaskin M et al (2008) Gout in the UK and Germany: prevalence, comorbidities and management in general practice 2000–2005. Ann Rheum Dis 67:960–966
Luk AJ, Simkin PA (2005) Epidemiology of hyperuricemia and gout. Am J Manag Care 11:S435–S442
Briesacher BA, Andrade SE, Fouayzi H, Chan KA (2008) Comparison of drug adherence rates among patients with seven different medical conditions. Pharmacotherapy 28(4):437–443
Riedel AA, Nelson M, Joseph-Ridge N, Wallace K, MacDonald P, Becker M (2004) Compliance with allopurinol therapy among managed care enrollees with gout: a retrospective analysis of administrative claims. J Rheumatol 31(8):1575–1581
Harrold LR, Andrade SE, Briesacher BA, Raebel MA, Fouayzi H, Yood RA, Ockene IS (2009) Adherence with urate-lowering therapies for the treatment of gout. Arthritis Res Ther 11(2):R46
Solomon DH, Avorn J, Levin R, Brookhart MA (2008) Uric acid lowering therapy: prescribing patterns in a large cohort of older adults. Ann Rheum Dis 67(5):609–613
Zandman-Goddard G, Amital H, Shamrayevsky N, Raz R, Shalev V, Chodick G (2013) Rates of adherence and persistence with allopurinol therapy among gout patients in Israel. Rheumatology (Oxford) 52(6):1126–1131
Shalansky SJ, Levy AR (2002) Effect of number of medications on cardiovascular therapy adherence. Ann Pharmacother 36:1532–1539
Rozenfeld Y, Hunt JS, Plauschinat C, Wong KS (2008) Oral antidiabetic medication adherence and glycemic control in managed care. Am J Manag Care 14(2):71–75
Ho PM, Rumsfeld JS, Masoudi FA, McClure DL, Plomondon ME, Steiner JF, Magid DJ (2006) Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med 166(17):1836–1841
Cheong C, Barner JC, Lawson KA, Johnsrud MT (2008) Patient adherence and reimbursement amount for anti diabetic fixed-dose combination products compared with dual therapy among Texas Medicaid recipients. Clin Ther 30(10):1893–1907
Acknowledgments
We would like to thank the HSE-PCRS scheme for providing the data on which this study is based.
Conflict of interest
None
Author contributions
All authors contributed to the study design, analyses of the data and discussion and approved the final draft of the manuscript prior to submission.
Funding
The authors received a seed grant from the Research and Education Foundation at Sligo General Hospital to conduct the study.
Ethics approval
Ethics approval was attained from The Research Ethics Committee (REC) at Sligo General Hospital.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McGowan, B., Bennett, K., Silke, C. et al. Adherence and persistence to urate-lowering therapies in the Irish setting. Clin Rheumatol 35, 715–721 (2016). https://doi.org/10.1007/s10067-014-2823-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-014-2823-8