Abstract
Both rheumatoid arthritis (RA) and psoriatic arthritis (PsA) have a negative impact on patients’ quality of life (QOL). The aim of this study was to compare QOL and life satisfaction in patients with RA and PsA. Forty patients with PsA, 40 patients with RA, and 40 healthy control subjects were included in the study. Demographic data and clinical characteristics including age, sex, disease duration, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), peripheral pain assessed by visual analog scale (VAS) and Larsen scores of hand X-rays were recorded. Nottingham Health Profile (NHP) was used to evaluate QOL, and Life satisfaction index (LSI) was used to measure psychological well-being in both groups. The demographic data of the subjects were similar between the groups. The scores of all NHP subscales were significantly higher and the scores of LSI were significantly lower in PsA and RA patients than in control subjects. The inflammation markers including ESR, CRP, pain by VAS and Larsen scores were found to be significantly higher in RA patients. The scores of LSI were similar between the groups. Although the scores of physical domains of NHP (pain and physical disability) were statistically higher in RA patients (p<0.05), the scores of psychosocial subgroups of NHP were similar between RA and PsA patients (p>0.05). Both PsA and RA patients had disturbed QoL and decreased life satisfaction. In conclusion, peripheral joint damage, inflammation, and physical disability are significantly greater in RA but psychosocial reflection of QOL and life satisfaction are the same for both groups which can be explained by the additional impact of skin disease in patients with PsA.
Similar content being viewed by others
Introduction
Rheumatoid arthritis (RA) and psoriatic arthritis (PsA) are chronic inflammatory joint diseases associated with deformities and joint destruction. Psoriatic arthritis has previously been emphasized as a milder disease in terms of articular erosions than RA, but recently, it has become clear that PsA is much more aggressive than previously thought [1, 2]. PsA can be as severe as other arthropathies, leading to functional limitations and restrictions in individual’s lifestyle and disturbances in psychological well-being [1–3].
There has been a growing interest in the assessment of quality of life (QoL) particularly in chronic disabling conditions. Health-related QoL is a multidimensional construct reflecting patients’ subjective evaluation of the effects of a disease on their physical, psychological, and social functioning [4]. There is ample evidence that RA have a profound effect on patients’ functioning, QoL, and well-being [5–8]. QoL research in PsA is still in its early stages [4]. Knowledge of the exact comparative effects of RA and PsA on QoL and life satisfaction is limited in the literature [1, 2].
In recent years, a number of instruments have been used to assess health-related QoL and life satisfaction in chronic rheumatic conditions [9]. Nottingham Health Profile (NHP) is one of the best known and most widely used health-related quality of life instruments, that has been used in a wide range of diseases to assess subjective perception of physical, emotional, and social aspects of the illnesses [10–12]. The generic QoL instruments, including NHP, were previously reported as well established, reliable, and valid tools for psoriasis research [4]. A Turkish version of NHP has been developed and thoroughly tested for reliability and validity in Turkey [13]. Psychological well-being has previously been assessed by Life Satisfaction Index (LSI) in some chronic rheumatic conditions [14–16]. As far as we have known, there is no data about the life satisfaction status in patients with PsA in the English literature.
The aim of this study was to comparatively evaluate QoL and life satisfaction in patients with psoriatic and rheumatoid arthritis.
Materials and methods
The study group was comprised of 40 randomly selected patients with RA who had been followed at outpatient clinics of Physical Medicine and Rehabilitation (PMR); 40 randomly selected patients with PsA who had been followed at outpatient clinics of PMR and Dermatology and 40 healthy control subjects derived from hospital staff volunteered to take part in the study. Patients with RA fulfilled the revised American Rheumatism Association criteria [17] for RA. PsA was defined as an inflammatory arthritis with involvement of >1 joint, associated with psoriasis, and patients with PsA had to be rheumatoid factor negative. Patients with pure spondylotic involvement were excluded from the study. Demographic properties of the subjects including age, sex, years of education were obtained. Disease duration of the patients with RA and PsA was recorded. Severity of joint pain by visual analog scale (VAS), number of tender and swollen joints, erythrocyte sedimentation rate (ESR), levels of C-reactive protein (CRP) and modified Larsen scores of hand X-rays [18] were recorded as clinical and laboratory activity parameters in both patient groups. The severity of skin disease was assessed by psoriasis area severity index (PASI) [19] in patients with PsA.
The Turkish version of NHP [13] was used to assess QoL in patients and control groups. It is a self-administered questionnaire containing 38 items (answered yes or no) that measure six dimensions: energy (three items), pain (eight items), physical mobility (eight items), emotional reactions (nine items), sleep (five items), and social isolation (five items). Scores for each section can range from 0–100 with a higher score indicating more severely compromised QOL [13]. Life satisfaction index (LSI) [14] was used to measure psychological well-being in both patients and control subjects. LSI consists of 20 attitude items for which participants indicated whether they agreed, disagreed, or were uncertain. Scores could range from 0 to 20, with the greater value indicating maximum life satisfaction. The LSI is multidimensional in character and three factors are relish for life, mood tone, and congruence between desired and achieved goals. It has previously been used in chronic rheumatic diseases in Turkish population [15].
The scores of NHP and LSI were compared between patients and control subjects. The relationship between the scores of NHP and LSI and disease activity measures were analyzed in patients with RA and PsA.
Statistical analyses
Demographic properties of all subjects and characteristics of disease activity were summarized by descriptive statistics. One way analysis of variance (Anova) was used to compare the scores of QoL and LSI between patients and control groups. Tukey’s honestly significantly different (hsd) test was used to define the difference between the groups. Spearman correlation matrix was used to correlate disease activity measures and scores of QoL and LSI in patients with RA and PsA. Statistical significance was determined at p<0.05.
Results
The study population consisted of 40 RA, 40 PsA, and 40 control subjects. The demographic and clinical properties of the subjects are shown in Table 1. There was no difference between the mean values of demographic characteristics of the three groups. The disease activity measures including ESR, CRP, peripheral joint pain assessed by VAS and Larsen scores were significantly higher in RA patients than in PsA group.
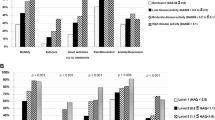
The scores of all NHP subscales were significantly higher and the scores of LSI were significantly lower in patients with PsA and RA than in control subjects (Table 2), indicating a poor quality of life and diminished life satisfaction in patients with RA and PsA. The scores of LSI were similar between PsA and RA patients. The scores of physical domains of NHP including pain and physical disability were statistically higher in RA patients than in patients with PsA. No statistical difference was found between the psychosocial subgroup scores of patients with RA and PsA, such as energy, sleep, social isolation, and emotional reactions.
There was a correlation between the physical domains of NHP and disease activity measures including the mean number of tender and swollen joints, pain by VAS, ESR, and CRP levels in patients with PsA. Psychosocial domains of NHP were also found to correlate with the mean ESR, CRP, and tender joint numbers in PsA patients. The scores of LSI were negatively correlated with pain by VAS scores and CRP values in the same group (Table 3). In addition, the mean score of PASI was correlated with the score of QoL domains including physical mobility and emotional reaction. In RA patients, the mean value of LSI was negatively correlated with pain by VAS scores and tender joint count. As expected, all disease activity measures but Larsen scores were correlated with physical domains of NHP including pain and physical mobility, while psychosocial domains of NHP were correlated with swollen joint, tender joint scores, and the scores of pain by VAS (Table 3).
Discussion
QoL measures reflect objectively the actual impact of a disease as an individual and the extent of the suffering [9]. Compromised QoL is invariably associated with functional disability, decrease in productivity and leads to some psychiatric disorders [4, 9].
In this study, we have evaluated the impact of PsA and RA on QoL and life satisfaction. The scores of LSI were lower and the scores of NHP subscales of RA and PsA patients were higher on all dimensions when compared with healthy subjects. RA patients had more dissatisfaction with their ability to participate in the domains that require physical efforts than the patients with PsA. Disease activity measures like pain, tender and swollen joint counts, ESR, and CRP were the most related factors for QoL for both diseases while CRP was the most related factor for life satisfaction for patients with PsA. The importance of disease activity, pain, and joint symptoms on QoL is not surprising in the RA group. As expected, articular involvement causes pain and leads to physical disability in this chronic condition.
Patients with PsA reported similar role limitations due to emotional problems but the scores of emotional reactions did not correlate with any of the disease activity parameters in our PsA group. Emotional reaction scores were found to be related with tender and swollen joint counts in RA group, indicating that they feel more dissatisfied with their social contacts when they have painful and swollen joints. Therefore, the disturbed QoL, especially in psychosocial domains, may be more related to additional skin problems rather than joint disease in patients with PsA.
QoL measures are widely used in dermatology and in psoriasis for the measurement of efficacy of medical interventions and as an outcome measure and demand for health services [20–24]. Zachariae et al. [22] investigated psoriasis-related QoL in a large sample of psoriasis. Approximately 30% of their patients had arthritis and patients with arthritis exhibited greater impairment of psoriasis-related QoL and greater self-reported disease severity for psoriasis. Lundberg et al. [23] measured health-related QoL with SF-36 in patients with atopic dermatitis and psoriasis. Their data indicated that patients with arthritis had significantly poorer QoL in both patient groups. Uttjek et al. [24] assessed determinants of QoL in patients with psoriasis and reported that large disease extent and joint symptoms were the strongest indicators for impaired QoL. All these results confirm that skin diseases associated with arthritis have an adverse impact on patient’s health-related QoL. But there is not much data on the extent of impairment of QoL and life satisfaction compared between patients with chronic disabling rheumatic conditions and patients with PsA.
Comparative researches on QoL and life satisfaction in patients with RA and PsA are limited in the literature [1, 2]. Sokoll and Helliwell [3] compared severity, disability, and QoL in patients with PsA and RA and concluded the same scores of function and QoL for both groups, despite the greater peripheral joint damage in patients with RA. Husted et al. [2] investigated health-related QoL between patients with PsA and patients with RA using the SF-36 health survey and health assessment questionnaire. Both of their patient populations experienced lower physical health compared with a general population sample, but there were some meaningful differences on how the two conditions affect health-related QoL. Although their patients with PsA reported higher levels of vitality, indicating a less disabling arthropathy, more role limitations and more bodily pain had been experienced by PsA patients than in patients with RA [1]. Similar to these studies, our data indicated that PsA patients had lesser disability than patients with RA; however, life satisfaction and impact of disease on psychosocial aspects of QoL was similar to RA patients, having a serious and progressive arthropathy. Subgroup analyses of NHP indicated that our patients with RA had significantly more problems with physical activities reflecting the greater damage and disabling condition in this patient group.
Although patients with PsA had less severe joint disease than in patients with RA, they scored similiarly in terms of life satisfaction and psychosocial aspects of QoL. A possible explanation for this may be the extent of skin disease. We found a significant correlation between the scores of PASI and scores of QoL domains including physical mobility and emotional reactions. Therefore, it is possible to mention the impact of additional skin disease on measures of QoL. Additional skin problems contribute psychosocial and physical disability. Severe skin disease may cause problems with self-esteem leading to disturbances in social contacts. Also, involvement of hand and genital areas may affect activities of daily living, self-care, and hygiene.
The impact of articular disease on health-related QoL is considerable. Additional skin problems in patients with PsA may cause a substantial physical and emotional toll on patients. It is important to quantify the patients’ perspective of the severity of their disease. In conclusion, although peripheral joint damage is significantly lesser in PsA than in RA, patients with PsA have impaired QoL and disturbed psychological well-being, similar to RA patients, which is related to the additional impact of skin disease in patients suffering from psoriasis. Current management strategies focusing on pain measures of articular involvement and cutaneous lesions will help to improve QoL and raise the life satisfaction in patients suffering from PsA.
References
Gladman DD, Antoni C, Mease P, Clegg DO, Nash P (2005) Psoriatic arthritis: epidemiology, clinical features, course and outcome. Ann Rheum Dis 64(suppl II):ii14–ii17
Husted JA, Gladman DD, Farewell VT, Cook RJ (2001) Health-related quality of life of patients with psoriatic arthritis: a comparison with patients with rheumatoid arthritis. Arthritis Care Res 45:151–158
Sokoll KB, Helliwell PS (2001) Comparison of disability and quality of life in rheumatic and psoriatic arthritis. J Rheumatol 28:1842–1846
de Korte J, Mombers FMC, Sprangers MAG, Bos JD (2002) The suitability of quality of life questionnaires for psoriasis research. Arch Dermatol 138:1221–1227
Coons SJ, Rao S, Keininger DL, Hays RD (2000) A comparative review of generic quality of life instruments. PharmacoEconomics 17:13–35
Wells G, Boers M, Shea B, Tugwell P, Westhovens R et al (1999) Sensitivity to change of generic quality of life instruments in patients with rheumatoid arthritis. OMERACT/ILAR task force on generic quality of life. Life outcome measures in rheumatology. International League of associations for rheumatology. J Rheumatol 26:217–221
Borman P, Çeliker R (1999) A comparative analysis of quality of life in rheumatoid arthritis and fibromyalgia. J Musculoskelet Pain 7(4):5–17
Sivas F, Erçin O, Tanyolaç Ö, Barça N, Aydoğ S, Özoran K (2004) The Nottingham Health profile in rheumatoid arthritis: correlation with other health status measurements and clinical variables. Rheumatol Int 24:203–206
Ortiz Z, Shea B, Dieguez MG, Boers M, Tugwell P, Boonen A, Wells G (1999) The responsiveness of generic quality of life instruments in rheumatic diseases. A systematic review of randomized controlled trials. J Rheumatol 26:210–216
Hunt S, McEven J, Mc Kenna S (1985) Measuring health status: a new tool for clinician and epidemiologists. J Roy Coll Gen Pract 35:185–188
Bostan EE, Borman P, Bodur H (2003) Functional disability and quality of life in patients with ankylosing spondylitis. Rheumatol Int 23:121–126
Coons SJ, Rao S, Keininger DL, Hays RD (2000) A comparative review of generic quality of life instruments. PharmacoEconomics 17:13–35
Küçükdeveci AA, McKenna SP, Kutlay S, Gürsel Y, Whalley D, Arasıl T (2000) The development and psychometric assessment of the Turkish version of the Nottingham Health Profile. Int J Rehabil Res 23:31–38
Neugarten BL, Havighurst RJ, Tobin SS (1961) The measurement of life satisfaction. J Gerontol 16:134–143
Çeliker R, Borman P (2001) Fibromyalgia versus rheumatoid arthritis: a comparison of psychological disturbance and life satisfaction. J Musculoskelet Pain 9:35–45
Bodur H, Borman P, Ozdemir Y, Atan C, Kural G (2005) Quality of life and life satisfaction in patients with Behçet disease: relationship to disease activity. Clinical Rheumatology 2005 Nov 3;1–5 (e-pub)
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS (1988) The American Rheumatism Association 1987 criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31:315–324
Larsen A, Dale K, Eek M (1977) Radiographic evaluation of rheumatoid arthritis and related conditions by standard reference films. Acta Radiol 18:481–491
Fredriksson T, Pettersson U (1978) Severe psoriasis—oral therapy with a new retinoid. Dermatologica 157:238–244
Mease PJ, Kivitz AJ, Burch FX, Siegel EL, Cohen SB et al (2004) Etanercept treatment of psoriatic arthritis. Arthritis Rheum 50:2264–2272
Kaltwasser JP, Nash P, Gladman D, Rosen CF, Behrens F et al (2004) Efficacy and safety of leflunomide in the treatment of psoriatic arthritis and psoriasis. Arthritis Rheum 50:1939–1950
Zachariae H, Zachariae R, Blomqvist K, Davidsson S, Molin L et al (2002) Quality of life and prevalence of arthritis reported by 5795 members of the Nordic psoriasis associations. Acta Derm Venereol 82:108–113
Lundberg L, Johannesson M, Silverdahl M, Hermansson C, Lindberg M (2000) Health-related quality of life in patients with psoriasis and atopic dermatitis measured with SF-36, DLQI and a subjective measure of disease activity. Acta Derm Venereol 80:430–434
Uttjek M, Dufaker M, Nygren L, Stenberg B (2004) Determinants of quality of life in a psoriasis population in Northern Sweden. Acta Derm Venereol 84:37–43
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Borman, P., Toy, G.G., Babaoğlu, S. et al. A comparative evaluation of quality of life and life satisfaction in patients with psoriatic and rheumatoid arthritis. Clin Rheumatol 26, 330–334 (2007). https://doi.org/10.1007/s10067-006-0298-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-006-0298-y