Abstract
Background and aims
The concurrent decrease in fat free mass (FFM) and increase in fat mass (FM), including central obesity, in patients with rheumatoid arthritis (RA) may be related to increased cardiovascular morbidity as well as to functional decline. The objectives of this study were to evaluate body composition and nutritional status in patients with RA and the feasibility of bioelectrical impedance (BIA) to detect rheumatoid cachexia.
Methods
Eighty RA outpatients (76% women), mean age 61 (range 22–80) years and with mean disease duration of 6 (range 1–52) years, were assessed by body mass index (BMI), waist circumference (WC), whole-body dual-energy X-ray absorptiometry (DXA), BIA and the Mini Nutritional Assessment (MNA).
Results
Fat free mass index (FFMI; kg/m2) was low in 26% of the women and in 21% of the men. About every fifth patient displayed concomitant low FFMI and elevated fat mass index (FMI; kg/m2), i.e. rheumatoid cachexia. BMI and MNA were not able to detect this condition. Sixty-seven percent had increased WC. Reduced FFM was independently related to age (p = 0.022), disease duration (p = 0.027), ESR (p = 0.011) and function trendwise (p = 0.058). There was a good relative agreement between DXA and BIA (FM r 2 = 0.94, FFM r 2 = 0.92; both p < 0.001), but the limits of agreement were wide for each variable, i.e. for FM −3.3 to 7.8 kg; and for FFM −7.9 to 3.7 kg.
Conclusion
Rheumatoid cachexia and central obesity were common in patients with RA. Neither BMI nor MNA could detect this properly. There was a good relative agreement between DXA and BIA, but the limits of agreement were wide, which may restrict the utility of BIA in clinical practice.
Similar content being viewed by others
Introduction
Rheumatoid arthritis (RA) is a chronic systemic inflammatory condition associated with reduced life expectancy [16]. Aberrations in body composition may contribute to the increased morbidity [25] as well as the mortality associated with RA. Cytokine-driven hyper metabolism and protein degradation linked to the disease causes reduction of fat free mass (FFM). Concurrently, there is often an increase in body fat mass (FM). This combined condition is called “rheumatoid cachexia” [23, 27]. The increase in FM [4], especially central obesity may add to CVD morbidity [16]. Data on waist circumference (WC) in RA patients are, however, sparse.
The reduction of muscle mass may have consequences for morbidity and functional capacity. Adults with medically well-controlled RA have 13–14% less body cell mass, i.e. FFM minus extracellular fluid and solids, than their matched controls [27]. This corresponds to one-third of the maximum survivable loss of body cell mass.
The prevalence of malnutrition, including rheumatoid cachexia, in RA varies with definitions, methods and populations, and is reported to range between 26 and 71% [5, 10, 11, 18]. Recently, we reported nutritional status and body composition measured by Mini Nutritional Assessment (MNA), the Subjective Global Assessment tool (SGA), the Malnutrition Universal Screening Tool (MUST), the Nutritional Risk Screening tool 2002 (NRS-2002), and dual-energy X-ray absorptiometry (DXA) in 60 in-ward RA patients with high disease activity and disability [7]. Reduced FFM was found in half of the women and in one-third of the men. The concurrent elevation of FM made BMI a non-reliable tool to detect this condition. Of the tested nutritional evaluation tools, the MNA was suggested to be used as a screening instrument for malnutrition, but because of its low specificity it was proposed to be complemented by body composition assessment [7]. Due to the fact that BMI is maintained by the parallel body cell mass decline and increase in body fat mass (FM), the identification of rheumatoid cachexia relies on measurement of body composition. There is a need to evaluate the feasibility of such measurement techniques in RA. DXA gives reliable information on body composition but is expensive and not mobile. On the other hand, bioelectrical impedance analysis (BIA) is a clinically easy available tool to assess body composition.
The purpose of the present study was to study body composition aberrations, i.e. rheumatoid cachexia and central obesity, and nutritional status in outward patients suggested to have lower disease activity than inward patients, and to evaluate the feasibility of BIA for the detection of rheumatoid cachexia in RA patients.
Patients and methods
Patients
Eighty consecutive outpatients, 61 women, with RA at the Rheumatology Department, Karolinska University Hospital Huddinge aged between 18 and 80 years (median 61 years) and with disease duration ≥1 year (median 6 years) were included in the study. The exclusion criteria were: current malignancy, severe cardiac insufficiency according to the New York Heart Association classification, i.e. NYHA > 3, severe renal failure, i.e. glomerulus filtration rate (GFR) <20 ml/min, chronic obstructive lung disease with emphysema, earlier gastric ulcer or intestinal surgery, known eating disorder or glucocorticoid injections within previous 2 weeks.
The study was approved by the Ethics Committee at the Karolinska University Hospital, with informed consent of the patients to participate, and was performed in accordance with the Helsinki declaration.
Methods
The patients attended the outpatient clinic after an overnight fast. They were asked to refrain from participation in strenuous exercise or consuming alcohol for 12 h before testing to avoid perturbation of hydration status. On arrival, each subject emptied the bladder and had weight and height measured immediately before assessment of body composition by BIA. Within 2 h body composition was assessed by DXA. Blood samples were analysed for erythrocyte sedimentation rate (ESR, mm/h) and serum albumin. The patients’ disease activity, function and MNA were assessed and they were questioned about weight change since onset of the RA disease.
Disease activity and function
The Disease Activity Score including 28 joints (DAS28) was used. DAS28 evaluates number of swollen joints, number of tender joints, the patients’ global assessment of health measured on a visual analogue scale (VAS, range 0–100 mm), and ESR. The DAS28 score ranges from 0 to 10 points, and 2.6 to 3.2 indicates low disease activity, >3.2 to ≤5.1 moderate and >5.1 high disease activity [21]. Functional status was measured using the Swedish version of the Stanford Health Assessment Questionnaire (HAQ), a self-reported instrument measuring capacity to perform activities of daily living [6]. The HAQ score ranges from 0 to 3, where a higher score indicates a higher degree of disability.
Anthropometry
BMI was calculated from weight/height2 (kg/m2). The subjects were weighed to the nearest 0.1 kg, and standing height was measured to the nearest 0.1 cm. In accordance with WHO standards, individuals with BMI values <18.5 kg/m2 were considered underweight, between 18.5 and 24.9 as normal, 25 and 29.9 as overweight and values greater than 30 indicated obesity [28].
To identify central obesity waist circumference (WC) was measured using a plastic, inelastic, flexible belt-type measuring tape. The subjects were standing and the waist was measured to the nearest 0.5 cm midway between the iliac crest and the lower rib margin. According to the International Diabetes Federation (IDF), a waist circumference less than 94 cm in men and 80 cm in women would be low risk; an intermediate risk is indicated by 94–101.9 cm in men and 80–87.9 cm in women. Values above 102 cm in men and 88 cm in women indicates an increased risk for developing type 2 diabetes, coronary heart disease or hypertension [2].
Body composition assessments by DXA and BIA
For whole-body DXA the GE-Lunar Prodigy, software enCore 2006, version 10, 20,105, Madison, USA, was used. Briefly, using specific anatomic landmarks, legs, arms, and trunk were isolated on the skeletal X-ray anterior view planogram using the DXA system’s automated software. The DXA software then provided compositional estimates of legs, arms, trunk, head, and whole body. Scans were performed with the subject wearing light indoor clothing and with no detachable metal objects present. DXA is considered a valid method to estimate body composition in RA patients [20]. The precision of soft tissue analysis for a Lunar Prodigy is 1% for FFM and 2% for FM [12].
BIA is based on the underlying principle that resistance or impedance to the flow of an electrical current through the body is dependent on three variables: the length of the conductive path, the volume of the conductive material, and the resistivity of the conductive material [13]. We used the BC-418 8-contact electrode system (Tanita Corp., Tokyo, Japan). It is designed to collect multiple sets of whole body and segmental impedance measurements without the need for placement of conventional gel electrodes. The system base has two foot-pad electrodes fastened to a metal platform set on force transducers for weight measurement. Each of the extremity hand-grip electrodes has an anterior and posterior portion. Hence, there are four separate foot-pad electrodes mounted on the system’s base and two electrodes in each of the hand grips. The eight electrodes are connected to a digital circuit board that electronically switches the electrical circuit under study. All measurements are carried out at 50 kHz with a 0.8 mA sine wave constant current. The measurements were carried out according to the manufacturer’s manual and performed by the same operator. The Tanita BC-418 produces results that are highly repeatable (less than 1% variation within itself) when used under consistent condition [15].
In both DXA and BIA FFM and FM were expressed in absolute (kg) as well as in relative terms (as percent of total mass). FFM can be expressed as total FFM or as appendicular FFM, i.e. arms and legs and it is the sum of lean body mass (LBM) and bone mineral. Since absolute FFM and FM are dependent of height, the fat free mass index (FFMI; kg/m2) and fat mass index (FMI; kg/m2) were calculated. An age and sex-matched European reference population, i.e. 2,982 men and 2,647 women from Switzerland, allowed us to classify our patients according to the body composition. About one-third of these individuals were of non-Swiss origin, so this reference population was suggested to be more representative of an European population than people of strictly Swiss nationality [24].
Cut-off values for low muscle mass were defined as FFMI values below the 10th percentile, corresponding to FFMI below 13.7–14.7 kg/m2 for women and 16.9–17.6 kg/m2 for men, depending on age. Obesity was defined as FMI above the 90th percentile, corresponding to FMI above 8.8–13.5 kg/m2 for women and 7.2–9.0 kg/m2 for men, also depending on age [24]. The desirable levels for FM% are 20–30% for women and 12–20% for men [1].
As there is no consensus about the cut of levels for rheumatoid cachexia, we decided to use the definition FFMI below the 10th percentile together with FMI above the 25th percentile [8].
Mini Nutritional Assessment
The MNA [29] (0–30 points) is composed of a dietary questionnaire, e.g. questions related to number of meals, food and fluid intake and autonomy of feeding, a subjective assessment, i.e. self-perception of health and nutrition, a global assessment, i.e. questions related to lifestyle, medication and morbidity and anthropometrical measurements, e.g. weight, height, and weight loss. MNA classifies individuals with adequate nutritional status (MNA > 23.5 points), with risk for malnutrition (MNA 17–23.5 points) and with malnutrition (MNA < 17 points).
Statistical analysis
Data were presented as mean (confidence interval, CI) or median (interquartile range, IQR) depending on the type of distribution. P values < 0.05 were considered significant.
T test for dependent variables, Spearman rank correlation analysis, and linear regression analysis were used to compare and evaluate body composition data from BIA and DXA.
The multiple linear regression models included at most five variables, due to the relatively small sample size. Before performing regression analyses, FFM, i.e. the dependent variable, was transformed by logarithm to obtain normality.
Analysis of variance was used to compare differences among the body composition values determined using the different techniques, i.e. BIA and DXA. The method of Bland and Altman [3] was used to assess agreement between BIA and DXA. The mean difference, in kg, between the methods (bias) and the ±2 SDs of the difference between methods (limits of agreement) were calculated. Ninety-five percent of the data points should be within the ±2 SDs of the mean difference.
The statistical analysis program STATISTICA 7, Stat Soft Scandinavia AB, was used for statistical analysis.
Results
Clinical characteristics of the RA patients are shown in Table 1. The patients had fairly low disease activity according to DAS28 and a good functional ability as registered by HAQ. All patients except two women were treated with disease-modifying drugs (DMARDs). One-fourth received TNF-blocking agents.
Body composition
Anthropometrical data of the patients are shown in Table 2. Both sexes reported a small median increase in weight since the onset of the RA disease. Mean BMI was in the overweight range. More than 20% of the women and 40% of the men were considered obese according to BMI [28]. A majority showed central obesity.
Body composition data as to FFM and FM according to DXA are presented in Table 3. FFMI was reduced, i.e. below the 10th percentile of the reference population, in 26 and 21% of the women and men, respectively. Rheumatoid cachexia, i.e. FFMI < 10th percentile and FMI > 25th percentile, was present in 18% of the women and 21% of the men, respectively.
Both absolute and relative fat mass was increased in both sexes. FMI indicated more subjects to be obese than BMI did, i.e. 31% of the women and 53% of the men had a FMI above the 90th percentile.
To elucidate the impact of the RA disease on FFM and FM correlation analyses were made between FFM and FM%, and age, gender, disease duration, DAS28, HAQ score as well as ESR. The clinical variables that were significantly correlated with body composition were used for multivariate analyses.
The multiple regression analyses with FFM as the dependent variable revealed female gender (p < 0.001), ESR (p = 0.011), duration of RA (p = 0.027), age (p = 0.022) and HAQ trendwise (p = 0.058) to be significantly and independently related with low FFM. Gender alone explained 65% of the variance in FFM, whereas the combined impact of the remaining four variables was 12%.
The multiple regression analyses with FM% as the dependent variable revealed female gender (p = 0.001) and ESR (p < 0.001) to be significantly and independently related with high FM. These two variables explained 30% of the variance of FM. ESR alone explained 21% of the variance in FM.
Treatment with biologics or glucocorticoids had no relation to body composition, data not shown.
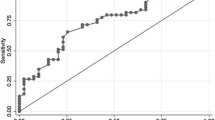
Comparison of body composition assessed by DXA and BIA
Compared with DXA, BIA underestimated FM by 2.2 kg and FM% by 4.3% and overestimated FFM by 2.1 kg, Table 3. However, there was a good relative agreement concerning all assessments of body composition between DXA and BIA (FM r 2 = 0.94, FFM r 2 = 0.92, both p < 0.001), Fig. 1.The limits of agreement were wide for each variable; FM −3.3 to 7.8 kg and FFM −7.9 to 3.7 kg, Fig. 2. The agreement between DXA and BIA was lower for appendicular muscle mass than for total FFM (data not shown).
Bland–Altman plot of differences between fat mass (FM) kg and fat free mass (FFM) kg determined by DXA versus BIA. Difference between methods calculated as DXA minus BIA values. Dotted middle line represents mean difference between methods (bias), and the outside solid lines represent the upper and lower limits of agreement (±2 SD of the mean bias)
Nutritional status
Among these outward RA patients MNA assessed one woman and none of the men as being malnourished (MNA < 17). Thirty-eight percent of the women and 16% of the men were considered as being at risk for malnutrition, Table 4.
Correlation analyses were made between MNA and WC, FFM, FM%, age, RA duration.
DAS28, HAQ score as well as ESR. The multiple regression analyses with MNA as the dependent variable revealed DAS28 (p = 0.007) and HAQ (p = 0.029) to be significantly and independently related with low MNA. These two variables explained 30% of the variance of MNA. DAS28 alone explained 25% of the variance in MNA.
Discussion
This study showed that patients with RA often displayed reduced FFM despite low disease activity. Thus, FFMI as estimated by DXA was below reference in 26% of the women and 21% of the men. These outpatients, like the inpatients we have reported on earlier [7], did not appear emaciated and they did not have anorexia. A concomitant increase in FM concealed this decrease in FFM. DXA provided evidence that the patient group could be assessed as obese as mean FM% was above the desirable levels for both women and men. FMI was above the 90th percentile in one-third of the women and in more than half of men.
The finding of low FFM together with stable or increased FM is in agreement with the concept of rheumatoid cachexia described by Roubenoff et al. [23]. However, the high frequency was somewhat surprising. Rheumatoid cachexia has been postulated to be associated with excess production of inflammatory cytokines and low physical activity [8, 22], but the RA disease in the present patients was fairly well controlled concerning inflammatory activity and physical function. A possible explanation is that the derangement of body composition is a result of several years of disease with varying, but elevated, inflammatory activity in combination with low physical activity. This assumption was supported by the negative correlations between FFM and disease duration as well as age and also between FFM and ESR and functional status (HAQ). Interestingly, FM% correlated significantly and positively with ESR. Adipose tissue is known to produce cytokines like TNF-α and IL-6 [9].
The majority of the present RA patients displayed central obesity as assessed by WC. Thus, our findings imply that one- and two-thirds of the females and males, respectively, were at risk for developing type 2 diabetes, coronary heart disease, or hypertension [2], whereas one-fourth of RA patients would be at intermediate risk for these conditions. The results highlights that the patients are not only at risk due to the chronic inflammation and loss of FFM. The extra burden of overweight and central obesity most likely also contribute to the known excess CVD mortality [16]. As the loss of FFM was not an isolated phenomenon but occurred in parallel with an increase of FM, BMI was not able to detect this kind of changes in body composition. This is in line with our previous report [7].
The use of DXA is suggested to be a fairly exact method to measure FFM and FM [13]. In the reference population, used here, FFM derived from BIA was validated against DXA in 343 of the healthy subjects between 18 and 94 years, with a BMI ranging from 17.0 to 33.8 kg/m2, with a bias of 0.03 ± 1.7 kg, r = 0.986. Thus, the cut-offs from this reference population should be valid, when using DXA as reference method. Percentile distributions are useful in determining whether or not an individual falls within the population range. Percentile ranks, such as the 10th and 90th percentiles, can be used to define nutritional depletion, muscle wasting and obesity [14].
The DXA method is considered sensitive to changes in body composition following weight gain or loss and changes related to ageing [17, 20]. DXA is, however, expensive and time-consuming. Other options for measuring body composition are therefore needed. We compared DXA with BIA and found a good relative agreement between the methods. However, in absolute terms BIA underestimated FM (% and kg) and overestimated FFM. Consistent with other reports [19, 25], we could also demonstrate wide limits of agreement between the two methods. Thus, although high correlation coefficients indicate good relative agreement, correlation analysis alone is not sufficient to verify the degree of coincidence among the methods [3]. Our findings are consistent with those reported by Volgyi et al. [30] when comparing DXA GE-Lunar Prodigy and Tanita BC-418. There was a systematic bias between the two methods (−2.1 kg for FFM and for FM +2.2 kg), which needs to be accounted for when BIA is used for assessing body composition in patients with RA.
BIA might prove particularly useful for the monitoring changes in body composition, for example, following new pharmacological treatments or physical activity interventions. In support of this assumption is the report by Thomson et al. [26] that the BIA method was valid for assessing changes in body composition in young obese women during weight loss.
A prerequisite for BIA to be valid in determining body composition is that the patients are not over hydrated. Therefore we made efforts in standardising the examination conditions as to hydration. Further, serum albumin was within normal range in these patients, which is in line with normal extracellular volume.
MNA was not able to detect reduced FFM among the present patients, which may reflect the fact that MNA is primarily developed to assess malnutrition among the elderly. Our results suggest that nutritional status, among RA patients, to a large extent is dependent on disease activity and function as shown here.
We conclude that patients with RA often have decreased FFM, are obese and display rheumatoid cachexia, even when assessed during periods when the disease is well controlled. These combined aberrations put RA patients at risk not only for cardiovascular and metabolic disturbances, but also for muscle weakness, infections, and disability [22, 27]. When assessing the RA patient in clinical practice it is of great importance to consider both body composition and nutritional status. Although BIA may overestimate FFM, BIA may be a feasible technique, and could be used together with WC and MNA to assess these conditions.
Abbreviations
- BIA:
-
Bioelectrical impedance analysis
- BMI:
-
Body mass index
- DAS28:
-
Disease activity score calculated on 28 joints
- DXA:
-
Dual X-ray absorptiometry
- FFM:
-
Fat free mass
- FFMI:
-
Fat free mass index
- FM:
-
Fat mass
- FMI:
-
Fat mass index
- HAQ:
-
Health Assessment Questionnaire
- MNA:
-
Mini Nutritional Assessment
- RA:
-
Rheumatoid arthritis
References
Abernathy RP, Black DR (1996) Healthy body weights: an alternative perspective. Am J Clin Nutr 63:448S–451S
Alberti KG, Zimmet P, Shaw J (2006) Metabolic syndrome—a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med 23:469–480
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW Jr (1999) Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med 341:1097–1105
Collins R Jr, Dunn TL, Walthaw J, Harrell P, Alarcon GS (1987) Malnutrition in rheumatoid arthritis. Clin Rheumatol 6:391–398
Ekdahl C, Eberhardt K, Andersson SI, Svensson B (1988) Assessing disability in patients with rheumatoid arthritis. Use of a Swedish version of the Stanford Health Assessment Questionnaire. Scand J Rheumatol 17:263–271
Elkan AC, Engvall IL, Tengstrand B, Cederholm T, Hafstrom I (2008) Malnutrition in women with rheumatoid arthritis is not revealed by clinical anthropometrical measurements or nutritional evaluation tools. Eur J Clin Nutr 62:1239–1247
Engvall IL, Elkan AC, Tengstrand B, Cederholm T, Brismar K, Hafstrom I (2008) Cachexia in rheumatoid arthritis is associated with inflammatory activity, physical disability, and low bioavailable insulin-like growth factor. Scand J Rheumatol 37:321–328
Hamdy O, Porramatikul S, Al-Ozairi E (2006) Metabolic obesity: the paradox between visceral and subcutaneous fat. Curr Diabetes Rev 2:367–373
Helliwell M, Coombes EJ, Moody BJ, Batstone GF, Robertson JC (1984) Nutritional status in patients with rheumatoid arthritis. Ann Rheum Dis 43:386–390
Hernandez-Beriain JA, Segura-Garcia C, Rodriguez-Lozano B, Bustabad S, Gantes M, Gonzalez T (1996) Undernutrition in rheumatoid arthritis patients with disability. Scand J Rheumatol 25:383–387
Kiebzak GM, Leamy LJ, Pierson LM, Nord RH, Zhang ZY (2000) Measurement precision of body composition variables using the lunar DPX-L densitometer. J Clin Densitom 3:35–41
Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Gomez JM, Heitmann BL, Kent-Smith L, Melchior JC, Pirlich M, Scharfetter H, Schols AM, Pichard C (2004) Bioelectrical impedance analysis—part I: review of principles and methods. Clin Nutr 23:1226–1243
Kyle UG, Piccoli A, Pichard C (2003) Body composition measurements: interpretation finally made easy for clinical use. Curr Opin Clin Nutr Metab Care 6:387–393
Manual Tanita BC-418 (2009) http://www.tanita.co.uk/index.php?id=95
Maradit-Kremers H, Nicola PJ, Crowson CS, Ballman KV, Gabriel SE (2005) Cardiovascular death in rheumatoid arthritis: a population-based study. Arthritis Rheum 52:722–732
Matarese LE, Steiger E, Seidner DL, Richmond B (2002) Body composition changes in cachectic patients receiving home parenteral nutrition. JPEN J Parenter Enteral Nutr 26:366–371
Munro R, Capell H (1997) Prevalence of low body mass in rheumatoid arthritis: association with the acute phase response. Ann Rheum Dis 56:326–329
Neovius M, Hemmingsson E, Freyschuss B, Udden J (2006) Bioelectrical impedance underestimates total and truncal fatness in abdominally obese women. Obesity (Silver Spring) 14:1731–1738
Podenphant J, Gotfredsen A, Engelhart M, Andersen V, Heitmann BL, Kondrup J (1996) Comparison of body composition by dual energy X-ray absorptiometry to other estimates of body composition during weight loss in obese patients with rheumatoid arthritis. Scand J Clin Lab Invest 56:615–625
Prevoo ML, van ‘t Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL (1995) Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum 38:44–48
Rall LC, Roubenoff R (2004) Rheumatoid cachexia: metabolic abnormalities, mechanisms and interventions. Rheumatology (Oxford) 43:1219–1223
Roubenoff R, Roubenoff RA, Ward LM, Holland SM, Hellmann DB (1992) Rheumatoid cachexia: depletion of lean body mass in rheumatoid arthritis. Possible association with tumor necrosis factor. J Rheumatol 19:1505–1510
Schutz Y, Kyle UU, Pichard C (2002) Fat-free mass index and fat mass index percentiles in Caucasians aged 18–98 y. Int J Obes Relat Metab Disord 26:953–960
Sun G, French CR, Martin GR, Younghusband B, Green RC, Xie YG, Mathews M, Barron JR, Fitzpatrick DG, Gulliver W, Zhang H (2005) Comparison of multifrequency bioelectrical impedance analysis with dual-energy X-ray absorptiometry for assessment of percentage body fat in a large, healthy population. Am J Clin Nutr 81:74–78
Thomson R, Brinkworth GD, Buckley JD, Noakes M, Clifton PM (2007) Good agreement between bioelectrical impedance and dual-energy X-ray absorptiometry for estimating changes in body composition during weight loss in overweight young women. Clin Nutr 26:771–777
Walsmith J, Roubenoff R (2002) Cachexia in rheumatoid arthritis. Int J Cardiol 85:89–99
WHO (1995) Report of a WHO expert committee, physical status: the use and interpretation of anthropometry. Technical report series, no 854, ISBN-139789241208543. http://www.who.int
Vellas B, Guigoz Y, Garry PJ, Nourhashemi F, Bennahum D, Lauque S, Albarede JL (1999) The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition 15:116–122
Volgyi E, Tylavsky FA, Lyytikainen A, Suominen H, Alen M, Cheng S (2008) Assessing body composition with DXA and bioimpedance: effects of obesity, physical activity, and age. Obesity (Silver Spring) 16:700–705
Acknowledgments
Supported by grants from The Swedish Rheumatism Association, King Gustav V 80 year’s foundation, Capio, Stig Thunes found, the Swedish Research Council and The regional agreement on medical training and clinical research (ALF) between Stockholm county council and the Karolinska Institute. All authors contributed practically and/or intellectually to this study, as to design, collection of data and analysing data as well as writing or giving input to writing the manuscript. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work has in part been presented at the Congress of American College of Rheumatology in San Francisco, October 2008.
Rights and permissions
About this article
Cite this article
Elkan, AC., Engvall, IL., Cederholm, T. et al. Rheumatoid cachexia, central obesity and malnutrition in patients with low-active rheumatoid arthritis: feasibility of anthropometry, Mini Nutritional Assessment and body composition techniques. Eur J Nutr 48, 315–322 (2009). https://doi.org/10.1007/s00394-009-0017-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-009-0017-y